Iliotibial Band Syndrome Causes, Symptoms, Treatment, Ayurveda Concept
By Dr Raghuram Y.S. MD (Ay) & Dr Manasa, B.A.M.S
Iliotibial Band is a thick band of fascia. It is formed by the fascia of the below mentioned muscles – gluteus maximus, gluteus medius and tensor fasciae latae. Iliotibial Band is abbreviated as ITB. It is proximally formed at the hip by this fascia.
The ITB runs from the hip to the knee cap. It runs along the lateral part of the thigh. It is also an important structure which is involved in the movements of your legs. The band gets inserted to Gerdy’s tubercle. It does not have any bony attachment along the femur bone. As a result it has a tendency to shift front to back as and when knee flexes and extends.
Read – Pratyangas: The minor organs, Definition, Number
The tract passes superficial to the Vastus Lateralis muscle and gets inserted mainly on the Gerdy tubercle of the lateral tibial plateau and also partially to the supracondylar ridge of the lateral part of the femur. The Iliopatella band is its anterior extension. It connects the lateral part of the patella (small bony prominence on the front of knee joint that you can feel). This prevents the medial translation of the patella. In between the ITB and lateral femoral epicondyle we can find a small recess. This space contains lateral synovial recess (a synovial extension of the knee joint capsule). Superior and inferior gluteal nerves supply ITB. The same nerves supply gluteus maximus and tensor fasciae latae.
The band is mostly made up of collagen fibres. Collagen being the strongest protein would allow better force absorption with weight bearing activities. In between the collagen layers small amounts of elastin fibres are also present. This would allow the band to be slightly elastic and pliable. This would help the band to act like a spring. In spite of this the band cannot be stretched like a muscle.
Read – Shaareera: Ayurvedic Study Of Anatomy And Physiology

Table of Contents
Functions of ITB
Proximally the band helps in extension, abduction and lateral rotation of the hip. Distally its functions depend on the knee joint position. The ITB lying anterior to the lateral femoral epicondyle is an active knee extensor and allows full extension to 20-30 degrees of flexion. The ITB lying posterior in relation to the lateral femoral epicondyle is an active knee flexor and allows 20-30 degrees of flexion to full flexion range of movements.
Read – Avascular Necrosis In Ayurveda – Causes, Symptoms, Treatment
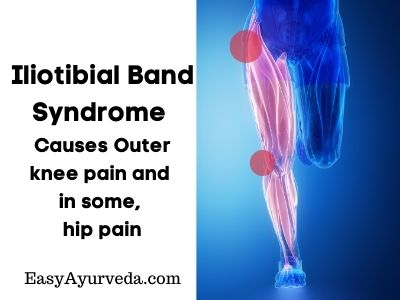
Iliotibial Band Syndrome (ITBS)
Iliotibial Tract Syndrome is one of the clinical conditions manifested as a result of ITB dysfunction. ITBS happens when the ITB gets irritated or swollen from rubbing against the hip or knee bones. It rubs against the bones when it gets too tight i.e. tensed.
It usually presents as sharp or aching pain on the outside of the knee or hip joint. This is due to a tight ITB. If the patient is an athlete experiencing these symptoms the diagnosis of iliotibial band syndrome is almost sure. This condition happens when the afflicted band which is swollen and irritated rubs against the mentioned bones of hip or knee. Many other symptoms can also be manifested due to swelling and irritation of the band. Physical therapy, medications or surgery (rarely) might help in easing the condition and these therapies are often used in combinations. ITBS can happen either in one leg or both legs. When it is present in both legs it is called bilateral ITBS.
Read – Effective Ayurveda treatments for Knee Osteo Arthritis (SandhiVata)
Risk factors
Young persons, especially those who exercise frequently are at higher risk for ITBS. Athletes most prone to this condition include cyclists, runners, skiers and those who play basketball, hockey or soccer. ITBS is most common in those who frequently exercise and in athletes. Ati vyayama i.e. excessive indulgence in exercises and sports are the most common and important causes for vata aggravation. On the other hand, vata aggravation in this band can cause ITBS.
Other risk factors –
- having bowed legs
- arthritis of knee joint / joints
- having one leg longer than the other
- weakness of muscles of hip joint, butt and abdomen
- rotating one’s ankle, leg or foot inward when they move
Read – Symptoms Of Vata Dosha Increase And Imbalance – Vata Vruddhi Lakshana
Incidence
- It is seen that ITBS is common in those undergoing training for U.S. Marines, at approximately 20% people.
- Frequent runners are more prone for ITBS, mainly long distance runners.
- ITBS accounts for about 12% of running injuries.
- More females have ITBS in comparison to males.
- ITBS is one of the many causes of knee pain and affects about 25% of adults.
Causes
When the ITB gets stretched too tight and rubs against the bone it would get irritated and swollen. Below mentioned are the possible causes of a tight ITB –
- Excessive foot pronation which stretches the ITB and brings it closer to the bones
- Weakness of the abductor muscles of the hip might tense up the ITB
- Internal tibial torsion wherein the shinbone is twisted inwards pulling the ITB closer to the bones
- Arthritis of the medial compartment of the knee joint which leads to a condition called genu varum which in turn pulls on your ITB making it tight
- Preexisting ITB tightness (if the condition persists since birth)
The ITB might also rub against your bones due to the below mentioned reasons –
- Pushing oneself too hard during exercise and doing it beyond capacity and limits
- Inadequate rest
- Not stretching enough before exercising
- Warming up too quickly before going into exercise
- Cooling down too fast after exercising
- Running on a curved or tilted surface / uneven surface
- Running downhill
- Wearing worn-out shoes
Read – Different Causes For Vata Dosha Imbalance, Increase
Symptoms of ITBS
The symptoms of ITBS are caused by a tense ITB. The symptoms of ITBS are as below mentioned –
Hip Pain – is caused due to the repeated rubbing of ITB on the greater trochanter in the hip. This friction causes inflammation in the tendon and hip pain along with a possible snapping sound in the joint.
Knee Pain – happens when your tense ITB rubs repeatedly against the lateral epicondyle as you flex and extend your knee joint. The friction causes inflammation in the tendon and knee pain.
Redness and warmth – can be observed on the outside of the afflicted knee joint.
Read – Classification Of Pain And Arthritis As Per Ayurveda
Nature of Pain in ITBS
The pain would start after your exercise at first. As the symptoms get worse the pain is felt entire course of the exercise. Eventually you would feel the pain while resting also. The initial pain of ITBS is often described as ‘aching and burning’. The more the exercise, the worse the syndrome and sharper the pain turns out to be.
Complications of ITBS
ITBS may cause PFPS (Patello Femoral Pain Syndrome) as a complication. In addition to the knee and hip pain the patient might also feel pain around and also under the kneecap (patella).
Prognosis of ITBS
Your ITBS might heal after rest, physical therapy and medications, usually a combination of all. Prompt treatment and skilful management is the key towards treating ITBS comprehensively.
When proper treatment, especially nonsurgical treatment is administered, improvement can be seen after about 4-8 weeks in about 50-90% people with ITBS. According to some studies improvement is seen within 2-6 weeks. Without treatment ITBS can worsen with time. Therefore the patient needs to speak to the healthcare provider about physical therapy, medications or other treatments which would work.
Read – Exercise Timing, Benefits, Side Effects, Ayurvedic Management
Diagnosis
History, examination and signs
The physician will reach a conclusive diagnosis of ITBS on the basis of the patient’s history and symptoms and after having conducted a complete physical examination. The doctor would check for the below mentioned signs too –
Crepitus – grating sounds / feeling when there is movement in knee or hip
Pain over the greater trochanter – in one or both hips
Pain over the lateral epicondyle – in one or both knees
Pain that increases along the length of your exercise
Pain gets worse when you go downhill
Tests to diagnose ITBS
The physician may carry out Noble and Ober tests to diagnose ITBS. Renne’s Test may also be conducted.
Related Video – Noble Test
Related Video – Ober Test
Related Video – Renne’s Test
The below mentioned imaging tests may also be required to reach at the correct diagnosis of ITBS –
MRI – helps in excluding other injuries like meniscal tear or lateral collateral ligament injury
Ultrasound – shows how your ITB moves when you flex and extend your hip or knee and thus helps in proving the presence of ITBS
Prevention
It is difficult to prevent this condition especially if you are a sportsperson or athlete. You may try changing the ways in which you do those activities so as to reduce the risk of ITBS. Examples are as mentioned below –
- Avoid running uphill or downhill or any slanted/uneven surface
- Manage right techniques in whatever activity you are indulged into
- Give enough time for your body to recover between workouts or events
- Shift your training intensity in a gradual way, speed up slowly when you are cycling instead of suddenly switching from slow to fast or from fast to slow
- Give plenty of time to properly stretch, warm-up and cool during exercising
- Slow down your warm ups and cool downs
- Stretch your IT band, hip muscles, thigh muscles and hamstring muscles often
- Alter your pattern of running, run with a shorter stride and flat surfaces
- Replace the shoes you wear regularly
- Wear supportive shoes
- Use foam roller to loosen up your IT band
Read – Sciatica – Ayurvedic Understanding And Successful Treatment Options
Treatment
Some treatments for ITBS can be done at home and other kinds of treatment might have to be done by an expert physician. Both these strategies shall be mixed skillfully to obtain better results.
The most common ITBS treatments include –
Rest – Rest your afflicted leg and do not indulge it in the exercise until the pain has gone away and ITBS has healed (according to some experts). Healthcare provider will guide the quantity of rest and activity you should undergo while under treatment.
Medicines for pain management – regular intake of NSAIDs including Ibuprofen and Naproxen. These medicines should be taken under medical supervision.
Manual therapy – this includes use of foam roller to massage body under the guidance and instructions of a physical therapist.
Physical therapy – you might have to practice certain effective stretches, strengthening exercises and other treatments to help relieve hip and knee pain under the guidance of a physical therapist. These help in lengthening ITB and also to decrease the tension therein. You will also be taught to warm up before exercise and cool down after exercise in better ways.
Posture Training – will help you to hold your body in a better during daily activities, playing sports etc.
Steroid injections – would reduce inflammation of ITB.
Surgery – is rare but might be recommended if medications and physical therapy doesn’t work.
Read – Ayurvedic Home Remedy For Sciatica, Rheumatoid Arthritis With Haritaki
Living with ITBS
The patients with ITBS would be worried so as to when they can get back to their normal activities. They can slowly get back to their regular activities once their pain has been relieved to a greater extent, of course with the permission and guidance of their healthcare provider. One can also make plans to deal with this condition and cope up with it. He or she shall also figure out what activities they can do and when to do them safely with the help of a healthcare provider. It is also important to know about the disease. If it is the first time one is experiencing hip or knee pain as per the description in ITBS one should contact their healthcare provider. They should immediately contact a healthcare provider or specialist especially when one doesn’t get better after a few weeks or gets even worse.
Prepare a list of signs and symptoms and queries which you need to discuss with doctor. The questions may be related to the causes, investigations needed, treatment and physiotherapy recommendations, need of surgery, preventive measures, dealing with the problem within home or about getting back to normal activities.
Best Yoga postures for ITBS
Gomukhasana – Cow Face Pose
Half cow pose – Ardha Gomukhasana
Ardha Matsyendrasana – Half Lord of the Fishes Pose
Uttanasana (variant) – Ankles Crossed Standing Forward Fold
Paschimottanasana (variant) – Ankles Crossed Seated Forward Fold
Agnistambhasana – Fire log Pose
Parivrtta Ardha Hanumanasana – Revolved Half Split
Parivrtta Trikonasana – Revolved Triangle Pose / Twisted Triangle
Parsvottanasana – Pyramid Pose
Uttanasana (variant) – Crossed Legged Wide Standing Forward Fold
Ardha Chandrasana (variant) – Crossed Ankle Standing Half Moon Pose
Kapotasana – Pigeon Pose
Supta Kapotasana – Reclined Pigeon Pose
Phalakasana (variant) / Vasishtasana – Plank with leg extension
Other poses
Anjaneyasana – Low Lunge / Kneeling lunge with a twist
Supta Hasta Padangusthasana – Reclining Hand-to-big toe Pose
Utthana Prishtasana – Lizard Pose
Shalabasana – Locust Pose
Jathara Parivritti – Revolved Abdomen Pose
Ayurveda Understanding Of Iliotibial Band Syndrome (ITBS)
We cannot directly find any condition resembling the clinical picture of ITBS in Ayurveda treatises. I have tried to compile the scattered references of conditions closer in explanation to ITBS. This will also be an understanding of this painful condition in comparison to different perspectives of the same as explained in the modern texts.
Effective Ayurveda treatments for Knee Osteo Arthritis (SandhiVata)
From anatomical and physiological perspective
The main functions of ITB are stabilisation of the pelvis and controlling the posture. Stability and posture maintenance are the functions of vata. Vata is invariably imbalanced in ITBS.
ITB is formed by collagen and elastin fibres which would allow it to be elastic and pliable slightly. Presence of collagen would also allow better force absorption when one is indulged in weight bearing activities. When vata dominates or is severely aggravated or in those of vata constitution who are prone for painful disorders, the collagen and elastin fibres lose their composition and integrity further leading to loss of elasticity and flexibility of ITB. Hardness and dryness in ITB occurs due to the same qualities of vata which are increased. This also reflects deterioration of kapha in these structures. Pitta may also be increased which worsens the picture in some conditions due to the onset and progression of inflammation. All these events lead to the manifestation of ITBS. On the contrary loss of elastin and collagen also may lead to vata increase.
Read – Symptoms Of Vata Dosha Increase And Imbalance – Vata Vruddhi Lakshana
From the perspective of pathogenesis of ITBS
The ITB is involved in causation of many movements in the hip and knee joints. Movements at the joints are caused by balanced vata and kapha (shleshaka type of kapha). When there occurs imbalance in these vata and kapha added with exposure to etiological factors like excessive exercise etc will predispose one to develop ITBS. Overall ITB dysfunction which causes ITBS is caused by vata aggravation.
Read – Exercise Timing, Benefits, Side Effects, Ayurvedic Management
From the perspective of etiological factors
- ITBS is most common in those who frequently exercise and in athletes. Excessive participation in exercises and athletics are therefore the main causes of ITBS. Ati vyayama i.e. excessive indulgence in exercises and sports are the most common and important causes for vata aggravation. On the other hand, vata aggravation in this band can cause ITBS.
- Other causes include bowed legs, having disproportionate lower limbs and inward rotation of ankle, leg or foot. Vata aggravation is responsible for all these conditions.
- Knee arthritis may also cause ITBS. Putting it in Ayurveda words, ITBS might be caused by aggravation of vata in the joints i.e. sandhigata vata.
- Too much tightening of ITB might be caused by vata aggravation. Excessive stretching of ITB and its rubbing against the bone can cause vata aggravation and this in turn causes symptoms of ITB which also seem to appear like symptoms caused by vata aggravation. Causes of ITB tightness explained above also are caused by vata aggravation. These include excessive foot pronation, weakness of hip muscles, internal tibial torsion, arthritis of knee joint etc.
- The causes due to which the ITB rubs against the bones also have a link with vata aggravation. Running on curved or tilted / uneven surfaces or downhill or wearing worn-out shoes might put the limb in untoward postures which are the chief causes for vata aggravation.
Read – OsteoArthritis Symptoms, Prevention, Lifestyle tips, Ayurvedic treatment
From the symptoms perspective
ITBS usually presents as sharp or aching pain on the outside of the knee or hip joint. This is due to a tight ITB. If the patient is an athlete experiencing these symptoms the diagnosis of iliotibial band syndrome is almost sure. Pain and tightness are features of vata aggravation. Vata is also aggravated by excessive exercise.
From the symptoms perspective the below mentioned conditions explained in Ayurveda can be considered as ITBS –
Uru sandhi shula / Uru sandhigata vata
Janu sandhi shula / Janu sandhigata vata
Other conditions which can be considered include –
Urushula
Vatarakta
Urugata Vata Prakopa
Nature of pain – Since the pain starts and gets aggravates along with and after exercise the clinical picture and appearance of symptoms mimics those occurring due to vata prakopa. We need to note that vata gets aggravated after excessive exercise as a rule. Aching and burning pain of ITBS suggests involvement of pitta also in the disease along with vata. Redness and warmth over the afflicted knee joint too reflects the involvement of pitta in the pathogenesis of ITBS. Crepitus is also present in the afflicted joint / joints. Shula i.e. pain and atopa i.e. crepitus along with swelling of the afflicted joints is the hallmark feature of sandhigata vata. PFPS which is a complication of ITBS also resembles sandhigata vata occurring in the knee joint.
Read – Growling Stomach Causes, Symptoms, Treatment, Ayurveda Concept
From treatment perspective
Even from the treatment perspective, the modern interventions for ITBS resemble the vata mitigating measures followed in Ayurveda. Rest, pain management, manual, physical and postural training all are anti-vata interventions.
Treatment of ITBS
ITBS shall be treated on the lines of –
- Vata chikitsa – treatment of aggravated vata is desired.
- Urugata Vata Prakopa – treatment of aggravation of vata in the thigh / thighs should be used.
- Pitta chikitsa – treatment of aggravated pitta should be done when signs and symptoms of pitta vitiation are found in ITBS.
- Sandhigata Vata Chikitsa – treatment of joints afflicted by aggravated vata – arthritis / osteoarthritis of joints fit into the treatment protocol.
- Uru sandhi shula / Uru sandhigata vata – pain in hip joint or arthritis of hip joint
- Janu sandhi shula / Janu sandhigata vata – pain in knee joint or arthritis of knee joint
- Snayugata Vata Chikitsa – treatment of ligaments / tendons afflicted by aggravated vata.
- Urushula – treatment of pain in the thighs should be considered.
- Vatarakta Chikitsa – treatment of simultaneous aggravation of vata and blood consequently afflicting the joints and soft tissues / treatment of gouty arthritis.
Treatments
ITBS shall be treated on the basis of predominant etiological factors and predominantly manifested symptoms. Below mentioned treatments would be highly effective in the treatment of ITBS.
External Therapies
- Abhyanga and Swedana – herbal oil massage and sudation on the afflicted joints (hip and knee) and thigh helps in relieving vata aggravation, pain, and tightness. It improves range of motions and enhances flexibility. These two therapies are usually combined for more effect.
- Among swedana – patrapinda sweda (leaf bolus sudation) help in relieving the symptoms of ITBS including pain and shashtika shali pinda sweda (medicated rice bolus sudation) helps in strengthening and supporting the joints.
- Dhara – stream pouring of warm medicated vata alleviating oils and milk should be used.
- Sthanika Vasti – oil pooling on afflicted joints i.e. hip (uru vasti) and knee (janu vasti) will help.
- Pichu – cotton pads / swabs dipped in vata mitigating oil is kept on the afflicted joints in line with ITB and bandaged if necessary.
- Lepa – anointments prepared with paste of vata / pitta mitigating herbs shall be applied on the afflicted parts.
- Upanaha – poultice prepared with paste of vata / pitta mitigating herbs and medicated oils shall be applied on the afflicted parts.
Internal Treatment
- Snehapana – oral administration of medicated fats (ghee / oil) in metered doses. If therapeutic purgation is planned to expel morbid pitta, medicated ghee is given in increasing doses over a period of 3-5 days or until the point of saturation is reached. Daily small doses of medicated fat (nitya sneha pana) too are helpful to mitigate vata and also to relieve pain and other symptoms.
- Virechana – therapeutic purgation is an ideal remedy for both vata and pitta aggravation. Unctuous purgatives shall be given in case of vata aggravation in ITBS.
- Vasti – enema with oil or ghee or both prepared with vata / pitta mitigating herbs is the best remedy for relieving symptoms of ITBS and also to alleviate vata.
Ayurvedic Medicines
Maharasnadi Kashayam
Sahacharadi Kashayam
Rasnasaptakam Kashayam
Gandharvahastadi Kashayam
Kokilaksham Kashayam
Guluchyadi Kashayam
Trayodashanga Guggulu
Rasnadi Guggulu
Mahayogaraja Guggulu
Kaishora Guggulu