Gastro intestinal Bleeding Causes, Symptoms, Differential Diagnosis
Article by Dr Raghuram Y.S. MD (Ay)
Gastrointestinal tract extends from mouth to the rectum. Gastrointestinal Bleeding includes bleeding in the gastrointestinal tract from mouth to rectum. This condition is also called as gastrointestinal haemorrhage or GI Bleeding or GI Bleeds.
Gastrointestinal bleeding itself is not a disease. It is a symptom or complication of some other disease.
The quantity of bleeding may range from significantly large amounts to small amounts. Significant blood loss over short time may present with vomiting of red blood or black blood, bloody or black stools, depending on the site of bleeding and passage of blood. Small amounts of bleeding over a long time may cause iron deficiency anaemia. Other symptoms may include abdominal pain, shortness of breath, pale skin, heart-related chest pain and passing out. Small quantum of bleeding may also go asymptomatic.
Table of Contents
Types of GI Bleeding
Gastrointestinal bleeding is broadly divided into 2 main types. They are:
Upper gastrointestinal bleeding – associated (caused by) peptic ulcer disease, oesophageal varices (due to cirrhosis of liver), cancer etc
Lower gastrointestinal bleeding – associated (caused by) haemorrhoids, cancer, inflammatory bowel disease etc
Causes
- Infections
- Cancers
- Vascular disorders
- Adverse effects of medications
- Blood clotting disorders
- OGIB (Obscure gastrointestinal bleeding) is a condition when a source is unclear following investigation
Signs and Symptoms
- Bleeding – As the name of the condition suggests, bleeding is the chief complaint (gastrointestinal bleeding is by itself a symptom). Bleeding can range from small non-visible amounts (detected by lab testing) to massive bleeding, wherein bright blood passes leading to shock. Rapid bleeding may cause syncope.
- Maelena – blood that is digested may appear black rather than red, resulting in ‘coffee ground’ vomit or tar coloured stool called maelena
- Feeling tired
- Dizziness
- Pale skin colour
Differential Diagnosis
Gastrointestinal bleeding can be divided mainly into 2 types i.e. upper GI bleeding and lower GI bleeding. Of all these, 2/3 of GI bleeds are from upper sources and 1/3 from lower sources.
Upper Gastrointestinal Bleeding
If the gastrointestinal bleeding occurs from a source between pharynx and ligament of Treitz, it is called upper gastrointestinal bleeding.
(Larynx – part of throat, behind the mouth and nasal cavity and above the oesophagus and larynx or voice box, they are the tubes going down to the stomach and the lungs
Ligament of Treitz or Suspensory muscle of duodenum – is a thin muscle connecting the junction between the duodenum, jejunum and duodeno-jejunal flexure to the connective tissue surrounding the superior mesenteric artery and celiac artery)
Upper gastrointestinal bleeding is characterized by haematemesis (blood vomiting) and melena (tarry stool containing altered blood).
The most common causes are –
- Peptic ulcer disease (PUD) – about half of upper GI Bleeds are due to PUD, about half of people with peptic ulcers have an H. Pylori infection
- Oesophageal inflammation
- Erosive disease
- Oesophageal varices – in those with liver cirrhosis, 50-60% bleeding is due to oesophageal varices
- Gastric ulcers
- Duodenal ulcers
- Mallory-Weiss tears
- Cancer
- Angio-dysplasia
- Medications – NSAID’s, COX-2 inhibitors, SSRIs, corticosteroids, anticoagulants, dabigatran, warfarin etc
Lower Gastrointestinal Bleeding
When the gastrointestinal bleeding occurs from the colon, rectum or anus, it is referred to as lower gastrointestinal bleeding.
It presents with passage of fresh red blood through rectum. Bloody vomiting will be absent unlike upper GI bleeds. Isolated melena may have its origin from anywhere between the stomach and the proximal part of Colon.
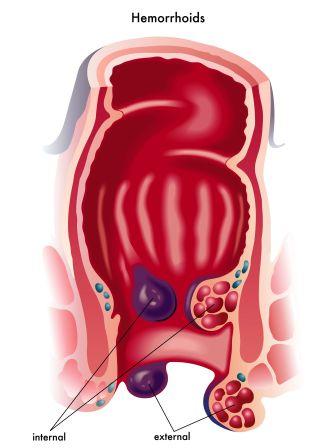
Common causes for lower GI Bleeds are –
- Haemorrhoids
- Cancer
- Angio-dysplasia
- Ulcerative colitis
- Crohn’s disease
- Aortoenteric fistula

Note: Bismuth and activated charcoal in medicines may turn the stools black. Blood from vagina or urinary tract may also be confused with blood in the stool.
Diagnosis
Diagnosis of GI Bleed is often based on direct observation of blood in the stools or vomit. This can be confirmed with a fecal occult blood test. Differentiating between upper and lower bleeding in some cases can be difficult.
Read related: Bleeding Disorders: Ayurveda Treatment, Diet, Home Remedies
Diagnosis of GI Bleeds consist of –
Thorough medical history
Physical examination
Blood tests – Laboratory blood tests includes cross matching blood, haemoglobin, haematocrit, platelets, coagulation time and electrolytes. If the BUN (blood urea nitrogen) to creatinine is greater than 30, the source of bleeding is more likely from the upper GI tract.
Faecal test for occult blood (small quantity bleeding) – Clots in the stool indicate a lower GI source for GI bleed. Melena stools suggest bleeding from upper GI.
Endoscopy of stomach, oesophagus and duodenum (upper GIT) to locate the area of bleeding
Endoscopy of the large colon
Medical imaging – for differential diagnosis
Blatchford score or Rockall score – The severity of an upper GI bleed can be judged based on these 2 scores. The Rockall score is the more accurate of the two.
Gastric aspiration and or lavage – A tube is inserted into the stomach via the nose in an attempt to determine if there is blood in the stomach.
Imaging – A CT angiography is useful for determining the exact location of the bleeding within the GIT. Nuclear scintigraphy is a sensitive test for detecting occult GI bleeding when direct imaging with upper and lower endoscopies are negative. Direct angiography allows for embolization of a bleeding source, but needs a bleeding rate faster than 1mL/minute
Prevention
Non-selective b blockers – reduce the risk of bleeding in people with cirrhosis or significant varices
EBL (Endoscopic band ligation)
pylori treatment – Prompt testing for and treating those who are H. pylori positive is recommended
TIPS (Trans-jugular intra-hepatic porto-systemic shunting) – to prevent bleeding in people who re-bleed despite other measures
Treatment
Resuscitation – includes intravenous fluids and blood transfusions. Blood transfusion is advised only when the haemoglobin (Hb) level is less than 70 or 80 g/L. Along with fluid resuscitation; airway management should also be taken care of.
Management of peptic ulcers:
- Crystalloid and colloids are believed to be equivalent for peptic ulcer bleeding
- Proton pump inhibitors (PPI) – can be administered orally or intravenously
- Tranexamic acid – inhibits clot breakdown
- Somatostatin and Octreotides – for variceal bleeds
For Variceal bleeding:
- Colloids or albumin
- Octreotide, vasopressin and nitroglycerin
- Telipressin
- Endoscopic banding or sclerotherapy
- Beta blockers and nitrates – to prevent re-bleeding
- Balloon tamponade – with Sengstaken-Blakemore tube or Minnesota tube
- Transjugular intrahepatic portosystemic shunt (TIPS)
- Oesophageal balloon (when other measures fail) – in those with persumed oesophageal varices
- Antibiotics – decreases the chance of re-bleeding in those who have cirrhosis and decrease mortality
Blood Products:
Gastrointestinal bleeding is said to be poorly benefited by blood transfusion. Some evidences have also proved transfusion to be harmful.
In cases of shock, O-negative packed RBCs are recommended.
If large amounts of packed RBCs are used, additional platelets and FFP (fresh frozen plasma) should be administered to prevent coagulopathies.
Blood transfusion should not be preferred in those having a haemoglobin level greater than 7-8 g/dL and moderate bleeding (even in those with pre-existing coronary artery disease)
Procedures
Blakemore oesophageal balloon – used for stopping oesophageal bleeding if other measures have failed
Placing nasogastric tube (upper GI Bleeds)
Endoscopy – is recommended to be done within 24 hours, many endoscopic treatments may be used like epinephrine injection, band ligation, sclerotherapy and fibrin flue (depending on what is found). Early endoscopy decreases hospital and the amount of blood transfusions needed. In high risk cases PPIs and hospitalisation for at least 72 hours are recommended.
Oesophageal balloon tamponade – may be attempted if other measures fail or not available
Colonoscopy – is useful for diagnosis and treatment of lower GI bleeding
Surgery – rarely used to treat upper GI bleeds, used in management of lower GI bleeds
Angiographic embolization – may be used for both upper GI and lower GI bleeds
TIPS is also useful in selected cases
Prognosis
- Death associated with GI bleed – is commonly due to other illnesses (some of which contribute to bleeding like cancer or cirrhosis)
- In all GI bleeding cases which are hospitalised, death occurs in 7% people
- Re-bleeding – despite treatment, re-bleeding occurs in about 7-16% cases (upper GI bleeding)
- In those with oesophageal varices – bleeding occurs in about 5-15% a year, if they have bled once, there is higher risk of further bleeding within 6 weeks
- pylori – Testing and treating for H. pylori can prevent re-bleeding in those with peptic ulcers
Epidemiology
- An upper GI bleed is more common than the lower GI bleed.
- Upper GI Bleed occurs in 50-150 per 100,000 adults per year.
- A lower GI bleed is estimated to occur in 20-30 per 100,000 per year.
- In USA, GI Bleeding results in about 300,000 hospital admissions a year.
- Risk of death from GI Bleed is between 5-30%.
- Risk of bleeding is more common in males and increases with age.
Just Before Finishing
Gastro Intestinal Bleeding is a dangerous scenario. The bleeding needs to be diagnosed and checked as early as possible. This article deals with information about the upper and lower GI Bleeding along with symptoms, complications, differential diagnosis and treatment from modern medicine point of view.
Click to Consult Dr Raghuram Y.S. MD (Ayu)








One comment on “Gastro intestinal Bleeding Causes, Symptoms, Differential Diagnosis”
Jyotirmoy sonowal
Dir sir lympho are curable in ayurvedic medicine I want to know