Hypercholesterolemia: Causes, Symptoms, Diagnosis, Prevention
Article by Dr Raghuram Y.S. MD (Ay)
Fat is an essential component of our body. It is an essential body building element, Ayurveda too sharing the same opinion. But anything in excess or less is bad to health. It will cause imbalance in the system. Fat is no exception.
Hypercholesterolemia is one such condition in which the body’s fat, that too bad fats are present in excess in the blood stream.
Table of Contents
Cholesterol
Cholesterol – It is a waxy, fat-like substance that is found in all the cells of the body. It is one of the lipids which manufactured by all animal cells and forms part of cell membrane. It is also the precursor of the steroid hormones and bile acids. It is obtained from foods that come from animals including egg yolks, meat, poultry, fish and dairy products.
It is a compound of sterol type found in most body tissues including the blood and nerves. Cholesterol and its derivatives are important constituents of cell membranes and precursors of other steroid compounds, but high concentrations in the blood promote atherosclerosis. High concentrations are mainly derived from animal fats in the diet.
Human body makes all the cholesterol that is needed to make hormones, vitamin D and substances that help to digest our food. It is also present in some of the foods that we consume. Cholesterol travels in our bloodstream (plasma) with protein particles in small packages called lipoproteins made up of both fat (inside) and proteins (outside).
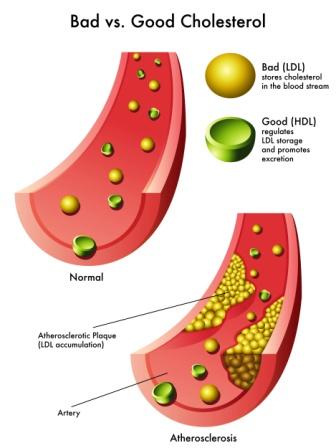
Cholesterol is carried throughout the body by 2 kinds of lipoproteins. They are LDL (low density lipoproteins) and HDL (high density lipoproteins). For good health, it is important that the body has healthy levels of both these lipoproteins.
Lipoproteins are classified by their density as:
VLDL – Very low density lipoprotein
LDL – Low density lipoprotein
IDL – Intermediate density lipoprotein
HDL – High density lipoprotein
LDL cholesterol is named as ‘bad cholesterol’. High level of LDL leads to build up of cholesterol in the arteries. Elevated levels of LDL cholesterol are associated with an increased risk of atherosclerosis and coronary heart disease.
HDL cholesterol is named as ‘good cholesterol’. Higher levels of HDL cholesterol are protective in nature. It carries cholesterol from other parts of the body back to liver. The liver removes the cholesterol from your body.
Hypercholesterolemia
Hypercholesterolemia means ‘high quantity of cholesterol in the blood’. It is a form of ‘high blood lipids’ and hyperlipoproteinaemia. High levels of LDL in the blood may be a consequence of diet, obesity, familial hypercholesterolemia (genetic diseases), diabetes or hypothyroidism
Other name – Dyslipidaemia
Signs and Symptoms
Hypercholesterolemia is most often asymptomatic. It doesn’t have its fixed set of symptoms. Most people with high cholesterol don’t have any symptoms until cholesterol-related atherosclerosis causes significant narrowing of the arteries leading to their hearts and or brains. The general symptoms are as said below:
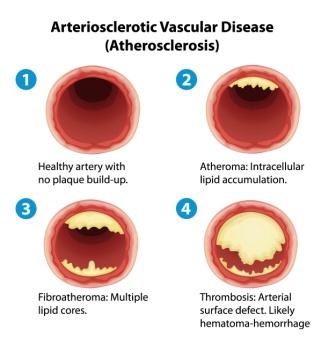
Atherosclerosis /arteriosclerosis – This is the most important symptom and presentation of hypercholesterolemia. It is caused by longstanding elevation of serum cholesterol.
What happens in atherosclerosis?
Serum cholesterol goes on accumulating in the arteries (the vessels or tubes that carry your pure blood to different part of the body from your heart). It may take several years to decades for threatening amounts of cholesterol to get accumulated in the blood vessels.
Atheromatous plaques – The elevated serum cholesterol levels in the arteries leads to the formation of atheromatous plaques.
These plaques cause progressive narrowing of the arteries involved thus hampering the free flow of blood.
Small plaques may rupture and cause a clot. The clot further obstructs to the flow of blood.
Heart attack – If such a block occurs in the coronary artery (blood vessels supplying the heart) it can cause heart attack.
Stroke – Similarly the blockage of an artery supplying the brain by a clot can cause a stroke.
Other symptoms and presentations of Hypercholesterolemia –
Tissue and organ ischemia – Gradual stenosis or occlusion causes diminished blood supply to the tissues and organs. As a result, the tissue and organ functions become impaired. Here tissue ischemia (restriction in blood supply) may manifest as symptoms. Example,
- Transient ischemic attack or TIA (temporary ischemia of the brain) manifests as temporary loss of vision, dizziness and impairment of balance, difficulty to speak, weakness or numbness or tingling. These symptoms are usually manifested on one side of the body.
- Ischemia of the heart may cause chest pain.
- Ischemia of the eye may manifest as transient visual loss of the eye, generally the affected eye.
- Ischemia to the legs may cause calf pain when walking.
- Ischemia in the intestines may present as abdominal pain after eating a meal.
Xanthelasma palpebrarum – manifests as yellowish patches of cholesterol deposits above the eyelids or underneath the skin around the eyelids. This condition is common in people with familial hypercholesterolemia (Type II a hyperlipoproteinemia).
Arcus senilis – white or grey discolouration of the peripheral cornea
Xanthomata – deposition of yellowish cholesterol-rich material of the tendons, especially of the fingers.
Type III hyperlipidemia – may be associated with xanthomata of palms, knees and elbows
Causes
Causes –
Hypercholesterolemia is usually a combined effect of environmental and genetic factors.
The environmental causes are:
Diet – diet has an effect on blood cholesterol. When the dietary intake of cholesterol is cut down, its production mainly in the liver typically increases (not always with total compensation) so that the reductions in blood cholesterol can be modest.
Obesity
Stress
The genetic causes:
Due to the additive effects of multiple genes
Single gene defect (ex, familial hypercholesterolemia)
Familial hypercholesterolemia affects about 1 in every 500 individuals
Secondary causes:
- Diabetes mellitus type 2
- Obesity
- Alcohol
- Nephritic syndrome
- Hypothyroidism
- Cushing’s syndrome
- Anorexia nervosa
- Monoclonal gammopathy
- Dialysis
- Medicines like thiazide diuretics, cyclosporine, glucocorticoids, beta blockers, retinoic acid
Diagnosis
Diagnosis basically depends on the biochemical tests conducted to know the range of cholesterol. Interpretation of cholesterol levels is done in the below said method –
| Total Cholesterol | LDL Cholesterol | HDL Cholesterol | |||
| Value | Interpretation | Value | Interpretation | Value | Interpretation |
| <200 mg/dL or
<5.2 mmol/L | Desirable | <100 mg/dL or
<2.6 mmol/L | Most desirable | <40 mg/dL or
<1.0 mmol/L | Undesirable, risk increased |
| 200-239 mg/dL or
<5.2 – 6.2 mmol/L | Borderline | 100 – 129 mg/dL or
2.6-3.3 mmol/L | Good | 41-59 mg/dL or
1.0-1.5 mmol/L | Okay but not optimal |
| >240 mg/dL or
>6.2 mmol/L | High | 130 – 159 mg/dL or
3.4-4.1 mmol/L | Borderline high | >60 mg/dL or
>1.55 mmol/L | Good, Lower risk |
| 160 – 189 mg/dL or
4.1-4.9 mmol/L | High and undesirable | ||||
| >190 mg/dL or
>4.9 mmol/L | Very High |
Family history of CAD, high cholesterol or diabetes will also help in clinching the diagnosis. Details regarding the diet we take or history of smoking might give good clue for doctor. The doctor may check for your BP and look for xanthomas and xanthelasmas. A simple blood test will be enough to trace the high level of cholesterol in your blood.
According to the guidelines established by the government-sponsored National Cholesterol Education Programme, the desirable level for LDL cholesterol depends on whether or not a person already has a disease caused by atherosclerosis or diabetes or other risk factors for CAD. In addition to a high level of LDL and diabetes, risk factors for CAD include:
- Being a male aged more than 45 years
- Being a female aged more than 55 years
- Being a woman with premature menopause
- Having a family history of premature CAD (father or brother younger than 55 with CAD or a mother or sister younger than 65 with CAD)
- Habit of smoking cigarettes
- Having high blood pressure
- Not having enough quantity of good cholesterol (HDL cholesterol)
If you have a CAD, peripheral arterial disease or have had a stroke from atherosclerosis, your LDL cholesterol should essentially be 70 mg/dL or less than that
The more the risk factors you have, the lower should be your target LDL cholesterol. LDL cholesterol levels of less than 100 are regarded as best, but less than 130 may be acceptable for people with no risk factors or have few of them.
The levels of HDL cholesterol also matters. People with levels below 40 mg/dL are more likely to develop atherosclerosis, heart disease and stroke. Levels of HDL cholesterol above 60mg/dL are associated with less atherosclerosis and are thought to help protect against heart disease and stroke.
Important features
For healthy adults, the UK National Service recommends upper limits of total cholesterol of 5 mmol/L and LDL cholesterol of 3 mmol/L.
For people at high risk of cardiovascular disease, the recommended limit for total cholesterol is 4 mmol/L and 2 mmol/L for LDL.
Higher levels of total cholesterol increase the risk of cardiovascular disease, particularly coronary heart disease. Levels of LDL or non-HDL cholesterol both predict future CHD.
The U.S. Preventive Services Task Force in 2008 strongly recommend routine screening for men 35 years and older and women 45 years and older for lipid disorders and treatment of abnormal lipids in people who are at increased risk of getting coronary heart diseases (CHD). They also have recommended routine screening for men aged 20-35 years and women aged 20-45 years if they have other risk factors for CHD. In 2016 they concluded that testing the general population under 40 years of age without symptoms is of unclear benefit.
In Canada, screening is recommended for men aged 40 and above and for women aged 50 and above. For those who have normal cholesterol levels, screening is recommended once in every 5 years.
Prevention
Availability of family history of high cholesterol, diabetes, CAD, stroke etc and their relation to high bad fats will press you to take preventive measures. Also having certain risk factors are the indicators to adapt the preventive measures and avoid the disease before it would have manifested. Even without the family history or risk factors, it is our duty to maintain discipline with respect to our food and lifestyle and take preventive measures against hypercholesterolemia because with the erratic lifestyle practices and undisciplined food patterns all of us are predisposed to this condition. Below mentioned are some of the preventive measures –
- Healthy and well balanced diet
- Regular on exercising
- Avoiding processed foods (containing saturated fats)
- Take good quantity of vegetables
- Take lot of fruits
- Take whole-grain breads and cereals
- Take low-fat dairy products
- Maintain a healthy weight
- Sip a glass of red wine every evening with dinner
- Eat small meals
- Avoid smoking
- Avoid foods containing high saturated fat
- Don’t consume butter, hard margarines, lard, fatty and processed meat, dairy fats
- Read related: 5 Things To Do After High Cholesterol Food Intake
Prognosis
On an average, diet and exercise can lower LDL cholesterol by about 10%. Medications can lower LDL by another 20% to more than 50%.
Epidemiology
In USA, the rates of high total cholesterol has been seen to come down from 17% in 2000 to 13% in 2010
Average total cholesterol in the UK is 5.9 mmol/L, while in rural China and Japan, average total cholesterol is 4 mmol/L.
Rates of CAD are high in Great Britain; the same is low in rural China and Japan.
More than 34 million American adults have elevated blood cholesterol levels (>240 mg/dL)
The most common inherited form of high cholesterol is familial hypercholesterolemia. This affects about 1 in 500 people in most countries. It occurs more frequently in certain populations like Afrikaners in South Africa, French Canadians, Lebanese and Finns.
Research
Many guidelines for clinical practice have detailed the hypercholesterolemia treatment
The National Cholesterol Education Programme revised their guidelines. Their 2004 revisions have been criticized for usage of non-randomized observational data.
In UK, the National Institute for Health and Clinical Excellence has made recommendations for treatment of elevated cholesterol levels, published in 2008
The Task Force for the management of dyslipidaemias of the European Society of Cardiology and the European Atherosclerosis Society published guidelines for the management of dyslipidemias in 2011
In diabetic population having hypercholesterolemia the ‘American College of Physicians’ recommends:
For all adults with known CAD and Type2 Diabetes, Lipid-lowering therapy should not be administered for secondary prevention of cardiovascular mortality and morbidity
In adults with type 2 DM and other cardiovascular risks, Statins should be used for primary prevention against macrovascular complications
People with Type2 DM should be taking at least moderate doses of statin, once lipid-lowering therapy is initiated
Routine monitoring of liver functions tests or muscle enzymes is not recommended (unless specified) for those people with Type2 DM on statins.
Medication
Medications should be considered in the treatment of hypercholesterolemia if the diet and lifestyle changes have been ineffective.
In these cases, Statins (HMG-CoA reductase inhibitors) are commonly used for treatment. They can reduce total cholesterol by about 50% in most people. They have also been said to be effective in decreasing the mortality in those who have had previous CVD. But the evidences are not strong enough. Statins may improve quality of life when used for primary prevention (in those without existing CVD).
Other agents are – fibrates, nicotinic acid and cholestyramine.
Injectable antibodies against protein PCSK9 can reduce LDL cholesterol and have been shown to reduce mortality.
If necessary, other treatments such as LDL apheresis or even surgery (for particularly severe subtypes of familial hypercholesterolemia) are performed.
Bile acid binding resins
Niacin
Selective inhibitors of intestinal cholesterol absorption, Example, Ezetimibe
Click to Consult Dr Raghuram Y.S. MD (Ayu)