Peptic Ulcers: Causes, Ayurvedic Treatment, Herbs, Home Remedies
Article by Dr Raghuram Y.S. MD (Ay)
Pain in the tummy is a common complaint. We all would have experienced it for a short time or for longer duration, sometimes like a passing affair and sometimes troubling our life activities, sometimes associated with food and lifestyle changes and many times without a reason. The nature and intensity of pain varies and depends on the causes leading to the manifestation of pain. Many pains are severe and chronic in nature; they are either constantly bothering you or intermittently visiting you every now and then. Pain which comes frequently and which stays for a long duration should not be ignored. It should be immediately brought to the attention of a doctor. Some pains may be life threatening.
Among many causes of chronic stomach or tummy pain, peptic ulcers or wounds (sores) occurring in your stomach or intestines take a lead. In this article we shall try to know about peptic ulcers, classification and symptoms of the same, medicines and treatment modalities from an Ayurvedic perspective.
Table of Contents
Peptic Ulcer
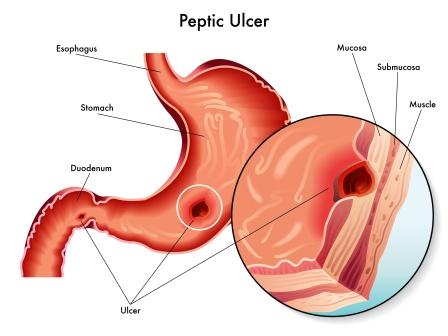
The term Peptic Ulcer is made up of 2 words,
Peptic – It refers to any part of the body that normally has an acidic lumen or is related to digestion or promotes digestion. The peptic areas of the human body are stomach and duodenum (first part of small intestine).
Thus in normal humans and in almost all humans, only the gastrointestinal tract is peptic.
Ulcer – means an open sore on an external or internal surface of the body (internal in this case), caused by a break in the skin or mucous membrane which fails to heal. Ulcers range from small, painful sores in the mouth to bedsores and serious lesions of the stomach or intestine.
Peptic ulcer – Thus Peptic ulcers are wounds or sores occurring in stomach or beginning part of the intestine. It is a common problem which occurs in the peptic areas of the body. These ulcers are most commonly caused by the bacteria and not by the acidic environment.
Preventive measures, home remedies
Preventive measures and Home Remedies
Timely food – The appetite is a signal of release of acids and want of food at that point of time, therefore we should attend the appetite immediately and provide food for the stomach
Avoid alcohol – totally avoiding alcoholic drinks or not drinking more than 2 alcoholic beverages in a day, alcohol should not be mixed with medicines
Avoid smoking, tobacco
Frequent hand wash – to avoid infections
Limit medicines – like ibuprofen, aspirin, naproxen sodium etc and other non-steroidal anti inflammatory drugs (NSAIDs)
Healthy lifestyle – use balanced diet rich in fruits, vegetables and whole grains
Don’t take food when you are thirsty and don’t drink water when you are hungry
Sleep well – maintain good quantity and quality
Avoid stress, anger and mood swings
Get body hydrated with good quantities of water regularly
Eat foods that are smooth on your stomach; avoid excessive salt, spices and sour foods, junks and refrigerated foods, stale foods etc
Home remedies for Peptic ulcers –
Fruits and Vegetables containing flavonoids (bioflavonoids) – Researches have shown that the below said fruits and vegetables having flavonoids may be helpful in healing peptic ulcers. They are:
Legumes, Soybeans, Apples, Green tea, Red grapes, Broccoli, Kale, Berries etc
Note: Some foods and drinks that contain flavonoids can irritate a stomach ulcer, example, citrus fruits, red wines etc
Yashtimadhu – Glyzyrrhiza glabra or Indian Licorice is an excellent remedy for ulcers.
- ¼ spoon of licorice powder should be taken with 1 spoon honey or 1 spoon melted ghee will heal the ulcers if taken for few weeks regularly.
- Milk boiled with licorice is also very beneficial in healing ulcers.
- Mix half teaspoon of licorice root powder in one cup of warm water. Cover it and leave it overnight. Next morning, add 1 cup of cooked broken white rice into the infusion and eat it. Take it daily for 1 week.
- Drink licorice tea 2-3 times daily for at least 1-2 week
- Chew and swallow 2-3 deglycyrrhizinated licorice (DGL) tablets thrice daily for a week
Foods containing Probiotics – are highly beneficial in ulcer healing. Probiotics are the living bacteria and yeast that help keep your digestive system healthy. They are present in the common foods which we consume, as listed below:
Buttermilk, Yoghurt, Miso, Kimchi etc
Probiotics are also available in the form of supplements.
Honey – Honey is one of the best options in the ulcer management. Ayurveda has used Honey as vehicle for many medicines used for healing shoola (colic caused by ulcers). Honey contains up to 200 elements including polyphenols and other antioxidants.
Take 2 tablespoons of raw honey daily, early in the morning on empty stomach.
Garlic – 6-8 cloves of garlic are smashed and boiled with 60 ml of milk and 240 ml of water and reduced until all the water evaporates and only milk (60 ml) is left over. The filtrate is consumed warm.
Learn how to do this here – Milk Garlic Home Remedy
Cranberry – People suffering from peptic ulcers can consume cranberry juice, eat cranberry or take its supplements.
Mastic – Mastic is the sap of a tree grown in the Mediterranean. Chewing mastic has shown to heal ulcers.
Take lot of fruits, vegetables and whole grains
Vitamin rich and polyphenol rich foods – are good to heal ulcers. Polyphenol rich foods and seasonings include:
Blueberries, Black olives, Dark chocolate, Mexican oregano, Dried rosemary etc
Avoid the below said to reduce ulcer pain:
Greasy and acidic foods, Spicy foods, Coffee, including decaf, Carbonated beverages, Chillies and hot peppers, Processed foods, Salty red meats, Deep fried foods, Milk
Other home remedies which have been tried to beat peptic ulcers
Cabbage & carrot juice: Slice half cabbage into small pieces. To this add sliced carrots, 2-3 in number. Put everything in a blender or mixer. Strain the ingredients to extract fresh juice. Take ½ to 1 cup of this juice before each meal. Make sure to prepare fresh juice each time. One cup at bed time also should be preferred.
Bananas: Bananas, both ripe and unripe varieties are very effective in ulcer healing. Eat at least 3 ripe bananas a day. Banana milkshakes are also good (provided you have milk tolerance). You can also try another method of eating bananas. Peel 2-3 bananas. Cut them into thin slices. Put these slices in the sun and dry them. After the banana pieces get dry, grind them into fine powder. Mix this powder and honey in the ratio of 2:1 (tablespoon measure). Take this mixture for about a week, 3 times a day.
Cayenne Pepper: Mix 1/8 th teaspoon of cayenne pepper in a glass of warm water. Drink it twice a day for the first 2 to 3 days. Gradually increase the amount of cayenne pepper up to ¼ teaspoon twice daily for the rest of the week. Pinch of cayenne pepper can also be added to soups, meats and other savoury dishes.
Coconut – is very beneficial to heal ulcers. It has antibacterial qualities; it kills the bacteria that cause ulcers. Coconut milk and coconut water have anti-ulcer properties. Drink a few cups of fresh coconut milk or tender coconut water daily. Also eat the kernel of the tender coconut. Alternatively, 1 tablespoon of coconut oil should be consumed for 1-2 weeks, 1 spoon in the morning and 1 spoon in the night.
Fenugreek – Boil 1 spoon of fenugreek seeds in 2 cups water, strain and drink after mixing ½ spoon honey. Alternatively, 1 teaspoon of fenugreek seed powder can be consumed with milk. Or 1 cup of boiled fenugreek leaves added with honey shall be consumed twice daily.
Slippery Elm: Take the inner bark of slippery elm and grind it into a powder. Mix 1 teaspoon of this powder in 1 cup of warm water. Drink this mixture 3 times a day for 1 week
Wood Apple: Soak 2-3 wood apple leaves in 1 cup of water in a copper vessel overnight. The next morning, strain the mixture and drink it on an empty stomach. Follow this treatment daily for few weeks to find relief from ulcer pain.
High fibre diet: Food containing high fibre such as oat, barley, lentils, carrots, beans, soya products is very good and effective in reducing the cause of the duodenal ulcers.
Chamomile / Dandelion tea: they are said to heal many infections, helps to keep your internal system clean and washes away any bacteria.
Vitamin A – Any fruit which is rich in vitamin A should be eaten regularly. Examples are watermelon, peaches, cabbages, oranges, blackberries and carrot juice. All these reduce the risk of duodenal ulcers. They can be taken in the form of juices, raw fruits, salads or as a snack. They should be properly washed before eating them.
Click to Consult Dr Raghuram Y.S. MD (Ayu)
Modern perspective
What is Peptic Ulcer or Peptic Ulcer Disease (PUD)?
Peptic Ulcer or Peptic Ulcer Disease (PUD) is a break in the inner lining of the stomach, the first part of the small intestine or occasionally the lower oesophagus (food pipe).
Ulcer in the stomach is called Gastric Ulcer
Ulcer in the small intestine is called Duodenal ulcer (first part of the small intestine which begins from the lower end of the stomach is called duodenum)
Common causes
Common causes for Peptic Ulcers –
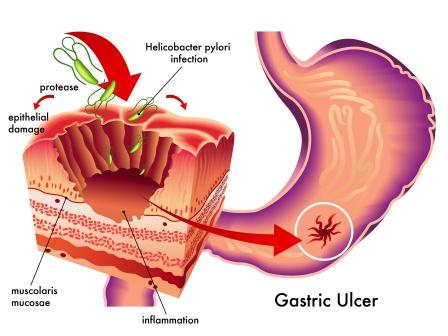
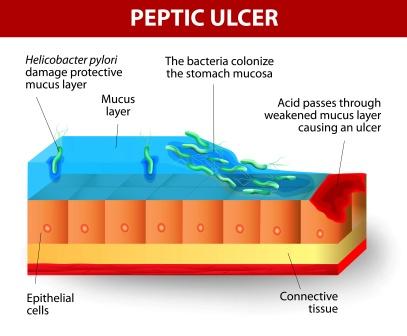
Bacteria, Helicobacter Pylori (H. Pylori) – it is a major causative factor of PU’s. 60% of gastric ulcers and 50-75% of duodenal ulcers are caused by H Pylori. This bacterium colonizes in the antral mucosa and causes chronic inflammation. Later due to failure of immune system to clear the infection, the bacteria cause chronic active gastritis (type B gastritis). Gastrin stimulates gastric acid production by parietal cells. In H Pylori colonization responses to increased gastrin, the increase in acid can contribute to the erosion of mucosa and subsequent formation of ulcer.
Drugs, Non-steroid Anti-inflammatory Drugs (NSAID’s) – example, ibuprofen (brufen) and aspirin
Stress – ulcers are caused due to stress, stress also may be due to serious health problems (stress ulcers), and chronic life stress could be contributory or triggering factor
Diet – excessive consumption of spices (minor contribution), caffeine and coffee, alcohol (increases risk when associated with H Pylori infection) are all considered contributory to PU’s
Habits – Smoking (when associated with H Pylori infection) and tobacco are contributory
Gastrinomas (Zollinger-Ellison Syndrome, ZE syndrome) – is a rare gastrin secreting tumour, will tend to cause multiple and difficult-to-heal ulcers
Other diseases: Behcet disease, Crohn disease, Liver Cirrhosis etc
Signs and symptoms
Common signs and symptoms of peptic ulcers:
Pain abdomen – epigastric pain (pain around the navel region) is characteristic of PU’s. The pain is correlated to time of intake of food. Duodenal Pain typically occurs about 3 hours after intake of a meal. The patient often wakes up at night with upper abdominal (tummy) pain; the pain is described as a burning type of pain or a dull ache. PUD also presents with upper abdominal pain which improves with eating (pain comes down when the person consumes food).
Bloating and abdominal fullness
Water-brash – excessive production of saliva is called water brash. This occurs as a defensive mechanism to buffer and dilute the acids coming into the oesophagus due to regurgitation of acidic contents of the stomach.
Belching
Nausea
Copious vomiting
Loss of appetite
Loss of weight
Haemetemesis – vomiting of blood usually occurs in PU’s due to bleeding directly from a Gastric Ulcer or due to the damage to the oesophagus from severe / continue vomiting
Melena – tarry, dark foul smelling faeces due to the presence of oxidized iron from haemoglobin
Gastric perforation or duodenal perforation – leading to acute peritonitis, and extreme stabbing pain is a rare condition related with PU. This condition requires to be managed by immediate surgery. This is a rare complication of improperly managed PU rather than a symptom.
Differentiating point – The time of the symptoms in relation to the meal helps in differentiating gastric ulcers and duodenal ulcers. A gastric ulcer would cause epigastric pain during the meal. Symptoms of duodenal ulcers would be initially relieved by intake of a meal, pain manifesting 2-3 hours after a meal.
Burning or gnawing feeling in the stomach area lasting between 30 mts to 3 hours commonly accompanies the ulcers. It can be expressed as hunger, indigestion or heart burn. Pain can be felt anywhere between navel region and sternum. It may last from few minutes to several hours and may be worse when the stomach is empty. The pain sometimes flares at night. Pain can be temporarily relieved by eating foods that buffer acid or by taking anti-acid medication.
Complications
Complications of peptic ulcer:
Gastrointestinal bleeding – bleeding due to erosion of blood vessels in stomach and duodenum
Perforation – formation of a hole in the wall of gastrointestinal tract (stomach and intestine walls). When this happens; the acidic contents of the stomach and duodenum spill into the abdominal cavity. This may lead to peritonitis (swelling or inflammation of the layers covering the abdominal viscera).
Penetration – it is a form of perforation in which the hole formed will lead to and the ulcer continues into adjacent organs such as the liver and pancreas
Gastric outlet obstruction – in this the pyloric canal gets narrow as an effect of scarring and swelling of gastric antrum and duodenum due to PU’s. This will often be associated with severe vomiting with or without bile.
Cancer – the GU’s which have occurred due to H Pylori are 3-6 times more likely to develop cancer of stomach
Diagnosis
Symptoms – Diagnosis of PU’s is mainly done on the base of clinical history and presentation of symptoms. Stomach or tummy pain (pain in the abdomen) is usually the first signal of a PU. PU is confirmed by either endoscopy or barium swallow. Diet is not contributory towards causing or preventing ulcers
A history of heartburn, GERD and use of certain forms of medication can raise the suspicion for PUD. Medicines associated with peptic ulcer include NSAID’s and most gluco-corticoids. In patients over 45 years of age with more than 2 weeks of the above mentioned symptoms, the odds for Peptic ulceration are high enough to warrant rapid investigation by EGD
Confirmatory tests – Endoscopy, Barium contrast X-rays (generally advised when symptoms don’t respond after few weeks of treatment or symptoms occurring for first time in people over 45 years with symptoms such as weight loss to rule out stomach cancer).
Esophago-gastro-duodenoscopy (EGD) or Gastroscopy
Blood tests (not reliable test)
Diagnosis of H Pylori –
- Urea breath test
- Direct culture from EGD specimen
- Direct detection of urease activity in a biopsy specimen by rapid urease test
- Measurement of antibody levels in blood
- Stool antigen test
- Histological examination and staining of an EGD biopsy
X-ray – Gas in the peritoneal cavity shown on an erect X-ray or supine abdominal X-ray is an omen of perforated PUD
Classification
Classification of Peptic ulcers
Depending on the area or organ afflicted, Peptic ulcers are classified as listed below:
Duodenal ulcer (occurs in duodenum or first part of the small intestine)
Gastric ulcer (occurs in the stomach)
Oesophageal ulcer (occurs in oesophagus or food pipe)
Meckel’s diverticulum ulcer (occurs in Meckel’s diverticulum)
Modified Johnson classification:
Type I: Ulcer along the body of the stomach, often along the lesser curvature at incisura angularis along the locus minoris resistantiae, not associated with excessive acidic secretion
Type II: Ulcer in the body in combination with duodenal ulcers, associated with excessive acidic secretion
Type III: Ulcer occurs in the pyloric canal within 3 cm of pylorus, associated with excessive acidic secretion
Type IV: Proximal gastro-oesophageal ulcer
Type V: Can occur throughout the stomach, associated with chronic use of NSAID’s (such as ibuprofen)
Differential Diagnosis
Gastritis: It is an inflammation or irritation of the stomach lining. It commonly presents with pain or discomfort in the upper abdomen. Burning, aching, gnawing or sore are the common words used to describe the pain or discomfort. Pain may be sharp, stabbing or cutting. Other symptoms include belching, nausea, vomiting, bloating, feeling of fullness or burning in the upper part of the belly etc.
Stomach cancer: It occurs when cancerous cells form in the stomach lining. It doesn’t cause symptoms until the later stages, so it’s often not diagnosed until it is more advanced.
Advanced stomach cancer is usually associated with the following symptoms: nausea, vomiting, frequent heartburn, loss of appetite, sudden weight loss, constant bloating, early satiety, bloody stools, jaundice, excessive fatigue, stomach pain etc.
Gastro-oesophageal reflux disease (GERD): It is a digestive disorder that affects the lower Oesophageal sphincter, the ring of muscle between the oesophagus and stomach. Heartburn also called acid indigestion is the most common symptom of GERD and usually feels like a burning chest pain beginning behind the breastbone and moving upward to the neck and throat. Many people say it feels like food is coming back into the mouth leaving an acid or bitter taste.
Pancreatitis: It is a disease in which the pancreas becomes inflamed. Pancreatic damage happens when the digestive enzymes are activated before they are released into the small intestine and begin attacking the pancreas. It presents with upper abdominal pain that radiates into the back. It gets aggravated by eating, especially fat rich foods. Other symptoms are swollen and tender abdomen, nausea, vomiting, fever, increased heart rate, weight loss, diabetes etc.
Hepatic congestion: It is also called congestive hepatopathy, nutmeg liver or chronic passive congestion of the liver. It is a liver dysfunction caused due to venous congestion, usually due to congestive heart failure. In addition to the heart and lung symptoms, there will be a sense of fullness and tenderness in the right hypochondriac region. Gastrointestinal catarrh is usually present and vomiting of blood may occur. Jaundice, ascites, generalized oedema, enlarged liver etc are other complaints.
Cholecystitis: is inflammation of gall bladder that occurs most commonly due to obstruction of the cystic duct by gall-stones arising from the gall bladder (cholelithiasis). It commonly presents with upper abdominal pain. Pain may radiate to the right shoulder or scapula. Nausea, vomiting and fever are commonly present.
Biliary colic: It is the term used to describe a tupe of pain related to the gallbladder that occurs when a gallstone transiently obstructs the cystic duct and the gallbladder contracts. Symptoms will be similar to cholecystitis.
Other conditions: Inferior myocardial infarction, Referred pain (pleurisy, pericarditis), Superior mesenteric artery syndrome etc.
Other points of interest –
A person with Gastro-oesophageal Reflex Disease (GERD) may have an acidic oesophagus (food pipe which carries food from mouth to stomach), particularly at the lower end.
A person with a Meckel’s diverticulum may have cells that produce acid within the diverticulum and therefore may be prone to peptic ulcers and or perforation of intestine.
Ayurvedic concept
Peptic Ulcers, Ayurvedic concept –
In Ayurveda, Peptic Ulcers can be correlated to Parinama Shula and Annadrava Shula. They are the subtypes of Shoola. Shula means pain or colic, used to describe abdominal pain to be precise.
Read related:
Parinama Shoola : Definition, Types, Treatment, Medicines
Annadrava Shoola: Definition, Treatment, Remedies
Yoga for Peptic ulcers
The below said Yoga postures are helpful in relieving and preventing Peptic ulcers:
Pranayama (set of breathing exercises), video:
Yogasanas for peptic ulcer treatment: (click on each Asana name to watch the video to learn it)
Bhujangasan (cobra pose)
Shalabhasana (Locust pose)
Uttanapadasan (Raised leg posture)
Pawanmuktasan (Gas release pose)
Balasana (Childs pose)
Shavasana (corpse pose)
Vajrasana (Diamond pose)
Padmasana (Lotus position)
Paschimottasana (Deep forward fold pose)
Supta virasana (Reclining hero pose)
Purvottasana (Upward plank pose)
Sethubandha sarvangasana (Bridge pose)
Ardha halasana (half plough pose)
Modern treatment measures
Treatment of Peptic ulcers, modern perspective
Acid reducing medications:
H2 antagonists or proton-pump inhibitors – decrease the amount of acid in the stomach, this helps ulcer healing
Young patients who have ulcer like symptoms are administered antacids or H2 antagonists
People on NSAID’s are given prostaglandin analogue to prevent ulcers
Treating H. Pylori –
2 antibiotics (example, clarithromycin, amoxicillin, tetracycline, metronidazole etc) and a PPI (proton pump inhibitor), sometimes with a bismuth compound
3 antibiotics (In complicated and treatment-resistant cases) example, amoxicillin + clarithromycin + metronidazole may be given with a PPI and sometimes with a bismuth compound
For uncomplicated cases – amoxicillin + metronidazole + pantaprozole
Surgery:
Perforated Peptic Ulcer is a surgical emergency. Most bleeding ulcers require endoscopy urgently to stop bleeding with cauterization, injection or clipping.
Research
Research and statistics related to Peptic ulcers:
Flavonoids are referred as ‘gastro-protective’ which means that they are good at defending and protecting the lining of the stomach and could also heal the ulcers. According to Linus Pauling Institute, there are no side effects of consuming flavonoids in the form of typical diet, but higher amount of flavonoids may interfere with blood clotting. Flavonoids are also available as supplements.
Declycrrhizinated Licorice (licorice with the sweet flavour extracted) – Studies showed that deglycyrrhizinated licorice might heal ulcers by inhibiting the growth of H. Pylori. It is available as a supplement. Excessive dosage might be bad for some people. Consuming more than 2 ounces daily for more than 2 weeks might worsen the existing heart problems or high blood pressure. Therefore it should be used with caution.
Studies have shown that probiotics may be helpful in wiping out H. Pylori and increasing recovery rate for the patients with ulcers.
Honey is a powerful antibacterial and studies have shown to inhibit H. Pylori growth.
Garlic extract – has shown to inhibit H. Pylori growth in lab, animal and human trials. Some people might not tolerate the smell and taste of garlic. They can preferably use garlic extract supplements. Garlic acts as a blood thinner. If you are taking garlic preparations you should keep your doctor intimated, especially when you are using warfarin or other prescribed blood thinners already.
Cranberry is known for its ability to fight urinary tract infections by preventing bacteria from settling on the walls of the bladder. Cranberry and its extract also may fight H. Pylori infections. Too much cranberry may cause stomach discomfort. It should be consumed in small quantities and gradually increased. Many commercial cranberry juices are heavily sweetened with sugar and / or high fructose corn syrup, which can also cause stomach upset and add empty calories. Such juices should be avoided.
Chewing mastic: Studies of the effectiveness of mastic on ulcers are mixed. One study shows that chewing mastic helps fight H. Pylori. You can chew the gum or swallow mastic in supplement form.
Polyphenol rich food: According to Mayo Clinic, a vitamin-rich diet can help your body heal your ulcer. Foods containing polyphenols, an antioxidant, can protect you from ulcers and help ulcers heal.
Cabbage – consists of lactic acid. Cabbage helps to produce an amino acid that stimulates blood flow to the stomach lining. This helps to strengthen the stomach lining and in the process to heal the ulcer. Cabbage also contains Vitamin C. Vitamin C is highly beneficial for patients with H. Pylori infections.
Fresh carrot juice – Experiments and studies have shown that carrot juice contains an anti-peptic ulcer factor (Vitamin U)
Banana – has some antibacterial compounds that inhibit growth of ulcer causing H. Pylori. Bananas also buffer and antagonize the acidity caused by gastric juices. They reduce inflammation and also strengthen the lining of the stomach.
Cayenne Pepper – the compound capsaicin present in cayenne pepper inhibits the secretion of stomach acids (review published in critical reviews in food science and nutrition). Apart from this it boosts the production of alkali and stimulates secretions and gastric mucosal blood flow thereby preventing and healing ulcers.
Licorice – helps the stomach and intestines to produce more protective mucus that forms a coating over the stomach lining. This in turn eases the pain from ulcers and speeds up the healing process.
Honey – An enzyme called glucose oxidase in raw honey produces hydrogen peroxide. This hydrogen peroxide kills harmful bacteria that cause ulcers. It also soothes and reduces the inflammation of the stomach lining.
Garlic – Researchers at the Fred Hutchinson Cancer Research Centre in Seattle discovered that the antibacterial and antimicrobial properties of garlic can keep levels of the H. Pylori bacterium in check, which contribute to the development of stomach ulcers.
Slippery elm – the inner bark of the slippery elm contains a good amount of mucilage that soothes and calms inflammation and pain. The mucilage helps remove excess fats in the intestines.
Wood Apple: Leaves of wood apple are used in the treatment of stomach ulcers. The tannins present in them protect the stomach against damage from secretion of excess acids. Juice extracted from wood apple fruit also helps reduce pain and inflammation due to its mucilage content.
Epidemiology
Epidemiology related to Peptic ulcers:
PU’s are present in around 4% population. About 10% of people develop a peptic ulcer at some point in their life
Lifetime risk for developing a peptic ulcer is approximately 10%. They resulted in 301,000 deaths in 2013 down from 327,000 deaths in 1990
In Western countries, the percentage of people with H. Pylori infections roughly matches age i.e. 20% at 20 years of age, 30% at 30 years of age and so on.
Prevalence in the 3rd world countries – 70% of population
Developed countries – around 40% prevalence
Transmission is by food, contaminated ground water and human saliva (kissing, sharing utensils etc)
Minority of cases of H. Pylori infection will eventually lead to an ulcer, larger population will get non-specific discomfort, abdominal pain or gastritis
PUD had a tremendous effect on morbidity and mortality until the last decades of 20th century. The reason that the rates of Peptic ulcer disease decreased is thought to be the development of new effective medications and acid suppressants and the discovery of the cause, H. Pylori.
The incidence of duodenal ulcers has dropped significantly during the last 30 years, while the incidence of gastric ulcers has shown a small increase, mainly caused by the widespread use of NSAIDs. The improved standard of living has also lowered the incidence of H. Pylori infections.
History
History related to Peptic ulcers –
The first description of a perforated PU was in 1670 in princess Henrietta of England
In 1958, a general practitioner in Greece named John Lykoudis treated patients for PUD with antibiotics
Helicobacter pylori were identified in 1982 by 2 Australian scientists, Robin Warren and Barry J. Marshall as causative factor for Peptic ulcers. They ruled our stress and spicy food theory in causation of Peptic ulcers.
In 1997, the Centres for Disease Control and Prevention launched a national education campaign to inform health care providers and consumers about the link between H. Pylori and ulcers.
In 2005, the Karolinska Institute in Stockholm awarded the Nobel Prize in Physiology or Medicine to Dr Marshall and his long time collaborator Dr Warren for their discovery of bacterium H. Pylori and its role in gastritis and PUD.
Treatment
Medicines to stop stomach acids – proton pump inhibitor (PPI), H2 blocker etc
H Pylori – Ulcers caused due to H Pylori are treated with combination of medications like amoxixillin, clarithromycin and a PPI (treatment might fail due to the antibiotic resistance on a rise)
Endoscopy and surgery – bleeding ulcers
Just before finishing,
Ayurveda has very good treatments, medicines and formulations, which have been time tested for comprehensively treating the Peptic ulcers vis-à-vis Parinama shoola or Annadrava Shula. There are innumerable simple formulations which can be prepared at home using kitchen ingredients as explained in the context of Shula treatment. But it is always wise to get diagnosed by a qualified Ayurvedic doctor in your vicinity, in an Ayurvedic way. The doctor will always be the best person who can prescribe you the right medicine or treatment. Many times the pain may have serious complications at the backdrop. The disease need and cause of pain should be differentially diagnosed in relation to other diseases which have similar presentation. The treatment and medicines for each and every person varies according to the nature of the ailment and constitution of the individual. It is always risky to self medicate.
Get your chronic pains treated and healed to their very best in a natural way, in an Ayurvedic way…but remember to take the consent of the doctor before trying any remedies!!!
Click to Consult Dr Raghuram Y.S. MD (Ayu) – email: drraghuramys@gmail.com








3 comments on “Peptic Ulcers: Causes, Ayurvedic Treatment, Herbs, Home Remedies”
Cook
Very thorough and informative! Thanks for your help! 🙂
aditya
can ayurvedic medicines treat ulcer or the infection(hpylori) in the stomach completely? i see that there are conditions mentioned in above post regarding resistant cases of infection so in such resistant cases how good do ayurvedic medicines work ? thanks. thanks for the informative post.
Dr J V Hebbar MD(Ayu)
Ayurvedic medicines with Panchakarma can be very useful in H Pylori.