Bone Mineral Density In Women: Staying Healthy With Strong Bones
By Gomathi Reddy.
She was frail, but happy.
The last time I saw her, she was smiling with a gentle wispy wave of her hand from behind the window – her last bye to me. A couple of weeks later, I got a call saying that she was in the ICU. I rushed to meet her, and was not allowed to. I heard the rest of the story from her relatives and domestic help – She’s been a chronic diabetic for years, and her Bone Mineral Density(BMD), as I ran through her reports, reported way below normal values – always. Apparently she was just walking in her backyard, had a gentle fall, got up and was attending to work at home as usual. A day later when the swelling in her ankle didn’t recede, she was asked to X-ray her leg and was diagnosed with a fracture. She was surprised. And then she had to undergo a surgery to get it back to shape. Because of her diabetes, the surgical incision wouldn’t heal, things got worse within a week, and here she was heading into a coma in the ICU. And within a week after that, she was gone. Those were the last few weeks in the life of another Indian woman who was a wife, mother, sister, daughter to her family and my favourite teacher at school.
These are stories that each one of us have – a few documented, a few reflected upon, a few taken in the stride – oblivious of the fact that all Indian woman, as they age, have a high risk of loss of bone or osteoporosis and rapid deterioration of BMD, leading to complications that are multiplied by the low-mineral intakes that we just overlook.
When Shakespeare wooed, “Frailty, thy name is woman,” I am sure he didn’t refer to an Indian woman with osteoporosis.
Table of Contents
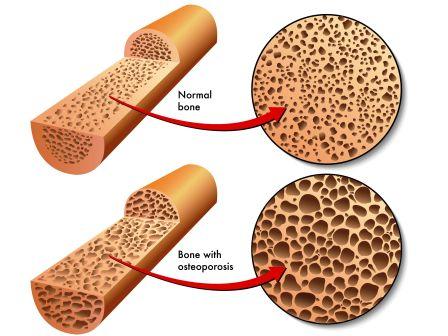
What is Osteoporosis?
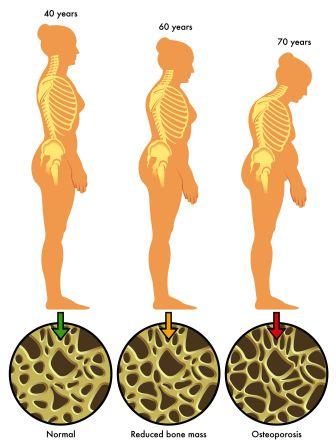
Osteoporosis is characterized by low bone mineral density with deterioration of bone tissue that leaves them fragile. The susceptibility to fracture is pretty high in such a situation. Studies point out that osteoporotic fractures in India occur commonly in both sexes, and may occur at a younger age than in the West, especially in women. Based on available data and clinical experience it is estimated that close to 25 million Indians with osteoporosis end up fracturing their wrists, hips, and spine. These fractures can limit their mobility, independence and emotional quality of their life.
Read related: Low Bone Density Causes, Ayurvedic Treatment, Diet
Bone degeneration causes
What causes degenerated bones?
Genetically the Bone Mineral Density for Indians is low compared to Caucasians(whites); our skeletal size is smaller and despite being a tropical country, we have poor exposure to sunlight, resulting in skin pigmentation and vitamin-D deficiency; Added to this is a calcium deficient diet, inconsistent or zero exercise – All these variables point to a bleak picture of poor bone metabolism and bone health in Indians.
Most Indian children start their adulthood with poor “Peak bone mass.” The maximum bone size and strength we attain at puberty, and at 30 is referred to as peak bone mass, of that stage.
For girls, the peak bone mass attained during puberty is an important indicator of how their bone mass would shape up as adults. Young girls should drink a lot of milk and get enough Vitamin D during these crucial years of their growth.
Children and adolescents form a lot of bone, resulting in denser, longer and heavier bones and appropriate skeletal growth. The rate of bone formation is much higher during these years, than its depletion (resorption). This formation and depletion continues through adulthood, though the pace of formation gets reduced. By the time Indians are 30, their peak bone mass for life is attained, post which it goes downhill. In this phase, depletion exceeds formation. Bone loss happens at 0.7 percent per year and in the case of women in menopause, bone loss happens at a rapid 2 – 7 percent per year.
This accelerated bone loss is highest in the vertebrae, which are cancellousor spongy bones. Most women suffer, because of bad posture or too much of domestic chores that leave their spines bent and mauled. In rural India, women also work alongside their men in non-mechanized fields – sowing, reaping and threshing. In the dry and arid regions, women and girls walk long distances every day to fetch a few pails of potable water. To reduce their trips, they end up carrying more than what their shoulders and hips can carry in a trip. Every such daily chore takes a toll on the woman’s health and her bones. Rural India’s lifestyle issues include non-smoking tobacco usage, by both men and women, which leads to depletion of calcium and brittle bones, very early in life.
Other than the primary causes for damaged bones, medical conditions such as hypogonadism, thyrotoxicosis, Cushing syndrome, anorexia nervosa,malabsorption syndromes, chronic liver and renal diseaseand chronic inflammatory conditions like rheumatoid arthritis may lead to secondary osteoporosis.
Fortunately, there are many things we can do at every age to keep our bones strong and healthy.
Diet and lifestyle tips
How do I keep my bones healthy?
Make Calcium and Vitamin D part of your daily diet. Avoid alcohol, caffeine and quit smoking. Compliment this with regular exercise and the right nutrition. These are simple, safe and cost-effective methods of avoiding brittle bones, as you age. Latest studies show medication being successful in treating metabolic issues, and reversal of bone loss through bone forming medications.
Though loss of bone density is considered to be a “silent killer,” the good news is that, the situation can be corrected with the right nutritious food and exercise. Here’s a run-down on the must-have minerals:

Calcium: Calcium is a major building-block of our bone tissue, and our skeleton houses 99 per cent of our body’s calcium. The calcium in our bones also acts as a ‘reservoir’ for maintaining calcium levels in the blood which is essential for healthy nerve and muscle functioning.
The amount of calcium we need to consume changes at different stages in our lives. Calcium requirements are high during teenage years with the rapid growth of the skeleton, and during this time, our body’s efficiency in absorbing calcium from food is good. With age, however, the ability to absorb calcium efficiently declines, and that is why older women are recommended higher amounts of calcium.
Dietary sources of calcium include milk and other dairy products which are also good enough for your daily dose of protein and micronutrients necessary for bone and general health. Vegetables, like broccoli, kale, the pith of citrus fruits, carob, sesame seeds and bokchoy are good sources of calcium too. You should also add canned fish with soft, edible bones (the calcium’s in the bones!) such as sardines, pilchards and salmon; nuts – especially brazil nuts and almonds; some fruits such as oranges, apricots and dried figs; and calcium-set tofu are a good mix to add to your dietary table. Homemade bone broth is also a good source of calcium. Add a few drops of vinegar to the broth and you can add this to soups or slurp it as is. The top layer or skin that is formed as the broth cools down has many nutrients and healthy fats.
There are also calcium-fortified breads, cereals, fruit juices, soy beverages and commercial mineral water with good amounts of calcium. These are an alternative route for lactose-intolerant and for vegan vegetarians to consume, for their daily dose of calcium.
If you are planning on taking supplements consult with your doctor on the appropriate dosage for you.
Vitamin D:
Next to calcium, Vitamin D builds your bone density by helping your intestines absorb your calcium intake. You can get your daily dose of Vitamin D with exposure to Sun i.e. Sun at around 7:30 – 8 am. If you in a location where there isn’t enough of Sun, take a vitamin D3 supplement.

Magnesium
Seaweed and green leafy vegetables like spinach and Swiss chard can be excellent sources of magnesium, as are some beans, nuts, and seeds, like pumpkin, sunflower, and sesame seeds, and avocados. If you opt for a supplement, choose magnesium threonate. It’s a newer type of magnesium supplement with superior ability to penetrate the mitochondrial membrane.
It is important to maintain a balance of your calcium with magnesium in the ratio of 1:1.
Vitamin K2:
Vitamin K2 is next only to Calcium and Vitamin D3 in its importance as far as maintaining healthy bone density is concerned. Vitamin K2 is the biological “glue” that plugs calcium into your bone matrix. It helps to move calcium into your bones and teeth and helps to remove calcium from your arteries and soft tissues.
When you take Vitamin D3, your body creates proteins which are K2-dependent. In other words you need K2 to activate these proteins to move the calcium around your body. If you do not have sufficient K2, then even if you have enough calcium in your system, it is not distributed appropriately. Infact it can lead to weaker bones and hardened arteries.
A good natural source of Vitamin K2 is fermented vegetables. Alternatively, you always can rely on vitamin K2 supplements.
The other minerals you should look out for are, Omega-6 and Omega-3 fats. Apart from these minerals, the body needs consistent exercise.
Make sure that your fitness program offers sufficient weight bearing activities for muscular strength, high intensity exercises for burning fat, and a couple of rounds to improve your cardiovascular fitness. Yoga can be a great way to regain bone strength and maintain hormonal balance.
Awareness about how to maintain a healthy bone density, across the various stages in a woman’s life can ensure a healthy and worry-free life as you get older.
Get Aware – Prevention is better than cure
The adage “prevention is better than cure” cannot be far from being true, when it comes to maintaining bone strength in women. Understand your basic bone structure and strength, before you embark on fortifying it.
Indian women have smaller bones with a thinner cortex and small diameter. They are more vulnerable than Indian men to suffering from depleted bone density. While men are at a risk for bone depletion after 70 years, women start going downhill by the time they are 45. Here’s a quick gist of what to expect at different stages of woman’s life.
Growing girls: Girls attain half of their total body calcium by the time they begin puberty. A regular period is a sign of good health and sufficient production of estrogen, in girls. Estrogen improves calcium absorption in the kidneys and intestines. By the time they are 20 almost all of their peak bone mass is achieved. Peak bone mass gets affected, when girls attain early or late onset of puberty. Obesity can pace up the onset of puberty in some girls, in turn affecting their peak bone mass for life. Obesity can have varying effects on girls depending on their genetic makeup, nutrition and life style.
The nutritional demands during adolescence is heavy as the body adds maximum bones strength, builds height and attains 95% of the growth needed for an adult. Calcium and Vitamin D intake are crucial for the bone strength.
Adolescent boys and girls must get 1200 mg of calcium every day. A cup of yoghurt or orange juice and 3 cups of green leafy vegetablesare sufficient to get your daily dose, or you must have it through supplements.
Children can be encouraged to see the negative effects of beverages and carbonated drinks, which decrease calcium absorption in the intestines. A Vitamin D supplement along with calcium ensures that the calcium gets absorbed in the intestines.
Exercise and Examinations
Weight-bearing exercises during adolescence are essential to reach maximum bone strength. Team sports like soccer or basketball or daily routines like walking and running fall under this category. But too much of these activities can be harmful for a young woman’s body. With too much activity, the ensuing hormonal changes can cause menstrual periods to stop – a condition referred to as amenorrhea. This leads to an imbalanced estrogen and hence bone loss at a time when a girl’s body must be adding bone rapidly, to be relevant for the rest of her life. Discuss with your doctor, if you notice any changes or interruptions to the menstrual cycle during these years.
If you are already suffering from osteoporosis, get into a yoga regimen only if your physician approves the practice. When you want to try yoga, keep the following guidelines in mind, to reduce the risk of fractures, during a session. It would be a good idea to attempt yoga with a qualified trainer in private, rather than being part of group yoga classes, which may have a mix of all age groups. The intensity to want to keep up with the rest of the class is not a good idea, if you have been diagnosed with osteoporosis.
Yoga
Yoga – The Watch OutList
Yoga is considered as an effective medicine for common ailments such as period pain, mild back pain, digestive complaints, insomnia, upper back and neck and shoulder tension, high blood pressure, arthritis and osteoporosis.
Yoga instructor, Nanammal, in Coimbatore city of Tamil Nadu is 93 and is a proof that a lifetime’s dedication to yoga can help one stay flexible and healthy at any age. You can choose to like her, even now.
For those diagnosed with osteoporosis, keep the rhythm and movement of postures slow and steady.
- Avoid flexing the spine to stretch the back, stretch the legs, or strengthen the abdominal muscles. Instead lie-down, lift or move the legs, the head and shoulders to achieve the same effect.
- Avoid pulling yourself into a twist using your arms. Introduce rotation gradually, using slow movement, without force.
- If you are asked to arch backwards to open the front of the chest, then replace that by arm movements that gently open the chest, without working on your back. You can also go into a reclining position, place a rolled towel or soft pillow under the upper back, mimicking a supported backbend. This is useful for restoring posture.
- Watch your wrists since wrist fractures are very common in people suffering from osteoporosis. Avoid supporting bodyweight with your hands. Strengthen your wrist muscles through mudras, arm movements, or sustained arm positions.
- Building leg and hip strength through balancing postures and standing poses are good for stabilizing the bone density but are extremely dangerous without the support of a wall or chair. Always ensure that you have a supportive friend or a teacher by your side.
- Do not try the headstand or the shoulder stand. Instead try restorative postures, like legs-up-the-wall.
Now that you have an idea of what not to do, the following brief notes on age-wise analysis of the bone mass density will help you to arrive at a plan that can iimprove upon yours/your loved one’s bone health.
Between 20 – 30 Years
This is the age when your body reaches peak strength. You need a good amount of calcium and Vitamin D to realize peak bone density. Make sure you get atleast 30 minutes of brisk walk or jog for 5 days a week. Take up any muscle strengthening activities for 2-3 days a week.
This is also the phase when a woman’s body needs maximum nourishment as it gets ready for pregnancy and breastfeeding. Get the recommended calcium and Vitamin D as prescribed by your doctor without fail, as your baby in the womb, will start extracting calcium out of your (her mother’s) bones to build her own skeleton. If you don’t have enough of it, you will lose bone strength rapidly during pregnancy and during nursing years. A healthy diet and exercise, during and post breastfeeding years, will help a mother regain lost bone strength.
Between 30 – 50 Years
Remodeling is a natural body process by which your body is replacing old bone with fresh bone, on an ongoing basis, until you are 40. After that, less bone is replaced, implying that the lost bone is not being replaced at the same pace. From then on, you will be living with an older bone that has gone through the travails of life. Exercise, nutritious food, calcium and Vitamin D supplements are important to maintain muscle mass that help support the bone from getting weakened by falls.
Older Than 50 Years
Most women are going through their menopausal years (42-55 years) and doctors will recommend a slightly higher dose of calcium and vitamin D. There is a rapid loss of estrogen, and some women experience a rise in testosterone too. As you must be aware normally estrogen and testosterone are present in both men and women; while estrogen levels are higher in women, testosterone is higher in men. Any imbalances in estrogen and testosterone levels triggers physiological changes (like growth of facial hair, in women) and rapid bone loss. It is a fact that most women lose upto 40% of their inner soft and spongy bone and 10% of their outer hard bone by the time they are 45, increasing their risk of falls and fractures.
Consult with your doctor, if your period is irregular or if you experience signs of menopause. Get a, Bone Mineral Density (BMD) done. Your bone health is measured by a Dual Energy XRay Absorptiometry (DXA) test.
If your doctor suggests a Hormone Replacement Therapy (HRT) to prevent bone loss, be aware that taking estrogen long term, post menopause has been found to have many side effects including, increased risk of blood clots, stroke, heart attack, breast and ovarian cancers, gall bladder disease and in some cases dementia.
Conclusion
Dr.Robert Thompson in his book “The Calcium Lie,” proposes that one of the best practical alternatives in terms of supplementation is to use natural, unprocessed salts, such as Himalayan salt, as they are one of the best sources of a very wide variety of trace minerals. Himalayan Crystal Salt, contains all 84 elements found in your body! Use it to keep your body’s metabolism in shape.
Dr. Kate Rheaume Bleue in his work, “Vitamin K2 and the Calcium Paradox: How a Little Known Vitamin Could Save Your Life,” suggests that Vitamin K2 along with Calcium, Vitamin D, and magnesium works synergistically to promote strong, healthy bones. Making this part of your nutrition intake early on, can make all the difference to a healthier bone mass and a stronger body, even in old age.
Proper diet, regular sun exposure, and weight bearing exercises can prevent and treat weakening bones.Avoid processed foods and soda – these deplete the calcium in your bones and increase bone damage. By avoiding processed foods, you are choosing a healthier lifestyle as you’d be ditching refined sugars and processed fructose, which are one of the reasons for insulin resistance. These simple changes to your eating habits will provide you with a good potassium to sodium ratio, which is important for maintaining bone mass. Eat raw organically raised fresh vegetables. Try vegetable juicing, for spicing up your new menu.
Above all treat your body with respect, before it gets too damaged to respond to any treatment. Your body is given to you to achieve a purpose in this life time, it is your duty to take care of the core of it – your bones and skeleton – with care. Start your day with a silent prayer appreciating the body that was given to you, and for every few steps and a bite that you take through the day, remember to add some nourishment to your bones.
References
- Gupta AK, Samuel KC, Kurian PM, Rallan RC. Preliminary study of the incidence and aetiology of femoral neck fracture in Indians. Indian J Med Res 1967; 55 : 1341-8.
- Vaishnava H, Rizvi SNA. Frequency of osteomalacia and osteoporosis in fractures of proximal femur. Lancet 1974; 1 : 676-7.
- Sankaran B. Clinical studies: Incidence of fracture neck of femur and intertrochanteric fractures in three Delhi hospitals. In: Sankaran B, editor. Osteoporosis. New Delhi: South East Asia Regional Office, World Health Organization; 2000. p. 9-18.
- Keramat A, Mithal A. Risk factors for osteoporosis in urban Asian Indian women presenting for a preventive health check- up. 2nd Joint Meeting of the European Calcified Tissue Society and the International Bone and Mineral Society, Geneva, 2005, June 25-29.
- Jha R, Mithal A, et al. Pilot case control investigation of risk factors for hip fractures in the urban Indian population. 2nd Joint Meeting of the European Calcified Tissue Society and the International Bone and Mineral Society, Geneva, 2005, June 25-29.
- Mitra S, Desai M, Ikram M. Vitamin D receptor gene polymorphisms and bone mineral density in postmenopausal Indian women. Maturitas 2006; 55 : 27-35.
- Vupputuri M, Goswami R, Gupta N, Ray D, Tandon N, Kumar N. Prevalence and functional significance of 25- hydroxyvitamin D deficiency and vitamin D receptor gene polymorphisms in Asian Indians. Am J ClinNutr 2006; 83 : 1411-9.
- Mitra S, Desai M, Ikram M. Association of estrogen receptor a gene polymorphisms with bone mineral density in postmenopausal Indian women. Mol Genet Metab 2006; 87 : 80-7.
- Sachan A, Gupta R, Das V, Agarwal A, Awasthi PK, Bhatia V. High prevalence of vitamin D deficiency among pregnant women and their newborns in northern India. Am J ClinNutr 2005; 81 : 1060-4.
- Marwaha R, Tandon N, Reddy DR, Aggarwal R, Sawhney RC, Saluja B, et al. Vitamin D and bone mineral density status of healthy schoolchildren in northern India. Am J ClinNutr 2005; 82 : 477-82.
- Harinarayan CV. Prevalence of vitamin D insufficiency in postmenopausal south Indian women. Osteoporosis Int 2005; 16 : 397-402.
- Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D, Srinivasarao P, Sarma KVS, et al. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am J ClinNutr 2007; 85 : 1062-7.
- Goswami R, Gupta N, Goswami D, Marwaha RK, Tandon N, Kochupillai N. Prevalence and significance of low 25 hydroxyvitamin D concentrations in healthy subjects in Delhi. Am J ClinNutr 2000; 72 : 472-5.
- Arya V, Bhambri R, Godbole MM, Mithal A. Vitamin D status and its relationship with bone mineral density in healthy Asian Indians. Osteoporosis Int 2004; 15 : 56-61.
- Shatrugna V, Kulkarni B, Kumar PA, Rani KU, Balakrishna N. Bone status of Indian women from a low-income group and its relationship to the nutritional status. Osteoporosis Int 2005; 16 : 1827-35.
- Tandon N, Marwaha RK, Kalra S, Gupta N, Dudha A, Kochupillai N. Bone mineral parameters in healthy young Indian adults with optimal vitamin D availability. Natl Med J India 2003; 16 : 298-302.
Author Bio: Gomathi Reddy is a Marketing Communication professional with specific research interest in gender studies. She writes about issues that affect women – the physical, emotional and everything in between. As an online journalist she also writes about challenges that plague the Indian society and blogs on how to make her country a better place to live.
Read her blog and connect with her, here