Heel And Foot Arch Pain: Plantar Fasciitis Tips, Remedies
By Dr Raghuram Y.S. MD (Ay).
Our busy life has kept us on our foot and toes; we keep running from morning till evening without rest and don’t even have time to notice what our legs and feet are feeling?
We don’t focus much on the cause, nature and behaviour of the pain because we already have a remedy in the closet!!
We have never got time to think why the pain is so constant and frequent?
But what happens in between is – a small problem progresses to become a bigger damage and Sometimes it becomes too late to attend them. Some foot and heel pains have a long standing course and keep visiting us frequently.
Plantar Fasciitis is one of the common causes of foot arch and heel pain which can torture you for a long duration if you don’t take caution at the earliest and find a permanent remedy.
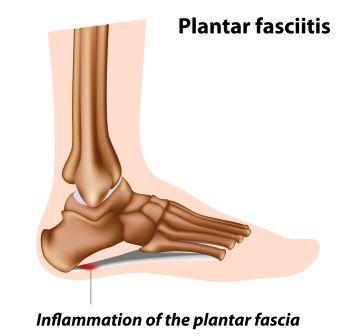
Table of Contents
Tips and remedies
Plantar fasciitis: Tips and remedies
Fill a tub with warm water. Add two tablespoons of salt in it.Soak your feet in it for about 20 minutes.
You can use sesame oil for massage as it has the ability to warm up the area and penetrates easily in to the skin.
In Plantar fasciitis, like in any other pain, the sooner you start the treatment, the sooner your feet will stop hurting you.
Being over –weight may cause or worsen it. Try these obesity tips and remedies.
Stop wearing footwear that does not fit your feet. Pick some good shoes which have good shock absorption, a good arch support and a cushioned sole. An athlete’s shoe will provide a cushioned sole and is comfortable during pain. Use heel cups or shoe inserts (orthotics). They will help to cushion your shoes. Use them in both shoes even if only one foot hurts. They are available in the athletic stores or drug stores.
Having tight Achilles tendons (tight tendons at the back of your heel), it may also cause plantar fasciitis. Hence, when you do oil massage with herbal oils such as Mahanarayana taila it helps to relieve foot arch pain, also do some massage over the back of the heel.
Having tight calf muscles also may cause foot arch pain. Hence, do not forget to massage your calves as well.
Consider wearing a soft comfortable foot wear especially if you have to stand for long hours.
Foot rest – Stop or minimise the activities that causes foot pain, avoid walking or running on hard surfaces
Icing the heel – Putting ice on your heel gives some relief, it reduces pain and swelling.
Contrast Baths: Use contrast baths with alternate hot and cold water. In some people, heat alone will make the symptoms worse. Therefore always end a contrast bath with a soak in cold water. If application of ice is not helping you after 2-3 days, try heat application such as a heating pad set on low heat.
Keep stretching – Toe stretches, calf stretches and towel stretches when done several times a day will be helpful. Doing these stretches when you first get up from the bed is essential.
Towel stretch – Pull on both ends of a rolled towel that you place under the ball of your foot. These stretches make your ligament more flexible and strengthen the muscles that support your arch.
Shoe morning – Put your shoes on as soon as you get out of your bed. Going barefoot or wearing slippers may make the pain worse
Splints: Try wearing splints at night as recommended by your doctor. Your doctor may advice you to use splints or may prefer injecting steroids in your heel or try some other alternative treatments when the above said do not work in your favor. Night splints gently stretch the fascia ligament and Achilles tendon and keep them from getting tight during the night.
Exercises for Plantar Fasciitis
Calf stretching in Bed:
- Take a towel or belt and loop it around the ball of your foot
- Keeping the leg straight, gently pull towards your body until you feel a stretch in the lower part of your leg
- Hold that for 30 seconds and repeat up to 5 times before taking your first step out of bed
Benefit:
- This exercise will help to loosen and relax the tight calf muscles whose pull on the fascia causes pain
Note: Do it early in the morning before getting out of your bed, to avoid the pain that your first few steps cause
Plantar Fascia Stretching:
- Pull your toes up with your hand until you feel a stretch along the ball of your foot.
- You may feel the stretch anywhere from the ball of your foot to your heel
- Hold this position for 30 seconds
- Repeat it for few times
Benefit:
- This exercise loosens up the tissues that are irritated
- Relieves pain
Calf stretching:
- Stand against a wall and slide one leg back, pushing the heel down towards the floor
- When you feel a stretch in the lower part of your leg, hold it for 30 seconds
- After 30 seconds bend your knees until a deeper stretch is felt a bit lower in the leg
- Again hold this stretch for 30 seconds and repeat this until you have done it 3 times on each leg
Benefit:
- By doing this exercise we will be stretching the 2 main muscles in the lower leg (calf) that attach to the heel
- By relaxing the tight calf muscles and Achilles tendon, the pain of plantar fasciitis is also relieved
Massage:
- Place a tennis ball on the floor
- Place your foot on the ball
- Gently roll the ball under your foot for a few minutes
- Put enough pressure on the ball to get a deep massage
- You may feel some soreness, but back off if you feel any pain
Massage tip video
Benefit:
- This exercise loosens up the plantar fascia, making it much less likely to become irritated
- Relieves pain
Ice massage:
- Fill water in a bottle and freeze it
- Keep the bottle filled with freezing water (just like the tennis ball in the above exercise) and roll it under your foot for 10 minutes, at the end of the day
- It is effective to keep away your inflammation in check while staying loose (after loosening your fascia with the ball roll)
Benefits:
- Reduces inflammation
- Keeps pain away
Note:
- These exercises will work and give relief but not instantaneously
- You need to practice them for a few weeks consistently
- See a doctor if you don’t see any improvement after making a sincere effort
Read related – 5 Free and Easy Solutions for Plantar Fasciitis
Wall push-ups or stretches for Achilles tendon:
- Face the wall
- Put both hands on the wall at shoulder height
- Stagger the feet (place one foot in front of the other)
- The front foot should be approximately 30 cm (12 inches) from the wall
- With the front knee bent and the back knee straight, lean into the stretch, (i.e. towards the wall) until a tightening is felt in the calf of the back leg, and ease off. Repeat 10 times
- Now repeat the exercise but bring the back foot forward a little so that the back knee is slightly bent
- Repeat the push-ups 10 times
- Do this exercise twice daily
Benefits:
- This exercise relaxes the tight calf muscles and Achilles tendon
Stair stretches for Achilles tendon and Plantar Fascia:
- Holding the stair-rail for support, with legs slightly apart, position the feet so that both heels are off the end of the step
- Lower the heels, keeping the knees straight, until a tightening is felt in the calf
- Hold this position for 20-60 seconds and then raise the heels back to neutral
- Repeat 6 times, at least twice a day
Benefit:
- This exercise stretches the tight Achilles tendon and plantar fascia
Yoga for Plantar Fasciitis
Utkatasana (Chair pose):
- Start off with Tadasana or mountain pose
- Keep your heels a little apart while your big toes touch each other
- Suck your lower belly inwards a little to support your spine
- Move your shoulder blades down and keep your chest open and thrust out across your shoulders
- Inhale and raise your arms perpendicular to the floor. Either keep the arms parallel, palms facing inward or join the palms
- Exhale and bend your knees, trying to take the thighs as nearly parallel to the floor as possible
- The knees will project out over the feet, and the torso will lean slightly forward over the thighs until the front torso forms approximately a right angle with the tops of the thighs
- Keep the inner thighs parallel to each other and press the heads of the thigh bones down towards the heels
- Firm your shoulder blades against the back
- Take your tailbone down toward the floor and in toward your pubis to keep the lower back long
- Stay for 30 seconds to a minute
- To come out of this pose, straighten your knees with an inhalation, lifting strongly through the arms
- Exhale and release your arms to your sides into Tadasana
Benefits:
- Strengthens the ankles, thighs, calves and spine
- Stretches shoulders and chest
- Stimulates the abdominal organs, diaphragm and heart
- Reduces flat feet
Video for Utkatasana
Adhomukha Svanasana – Downward Facing Dog pose
- Come onto the floor on your hands and knees
- Set your knees directly below your hips and your hands slightly forward of your shoulders
- Spread your palms, index fingers parallel or slightly turned out and turn your toes under
- Exhale and lift your knees away from the floor
- At first keep the knees slightly bent and the heels lifted away from the floor
- Lengthen your tailbone away from the back of your pelvis and press it lightly towards the pubis
- Against this resistance, lift the sitting bones toward the ceiling and from your inner ankles draw the inner legs up into the groins
- Then with an exhalation, push your top thighs back and stretch your heels onto or down toward the floor
- Straighten your knees but be sure not to lock them
- Firm the outer thighs and roll the upper thighs inward slightly
- Narrow the front of the pelvis
- Firm the outer arms and press the bases of the index fingers actively into the floor
- From these 2 points, lift along your inner arms from the wrists to the tops of the shoulders
- Firm your shoulder blades against your back, widen them and draw them toward the tailbone
- Keep the head between the upper arms, don’t let it hang
- Stay in this pose for 1-3 minutes.
- Then bend your knees to the floor with an exhalation and rest in the Child’s pose
Benefits:
- Calms the brain and helps relieve stress and mild depression
- Energizes the body
- Stretches the shoulders, hamstrings, calves, arches and hands
- Strengthens the arms and legs
- Relieves menstrual discomfort when done with head supported
- Helps prevent osteoporosis
- Improves digestion
- Relieves headache, insomnia, back pain and fatigue
- Therapeutic for BP, asthma, flat feet, sciatica, sinusitis
Read related – Downward-Facing Dog Pose
Adhomukha Svasasana video
Plantar fasciitis exercise videos
Stretch exercises:
Exercises:
Thai Massage:
Deep tissue myofascial release:
What is Plantar Fasciitis?
It is the most common cause of heel pain.
The plantar fascia is the flat band of tissue (ligament) that connects your heel bone to your toes. It supports the arch of your foot. When this plantar fascia gets strained, it gets weak, swollen up and irritated (inflamed). Then your heel or the bottom of your foot hurts when you stand or walk. It is often misspelt as plantar fasciitis.
Plantar fascia is a thick fibrous band of connective tissue that originates from the medial tubercle and anterior aspect of the heel bone. From here the fascia extends along the sole of the foot before inserting at the base of the toes and supports the arch of the foot.
Our foot has 2 surfaces – a dorsal surface (surface which you can see when you bend your head) and a plantar surface (surface of foot on which you walk i.e. which faces the floor)
Plantar Fasciitis is a painful condition occurs on the side which faces the floor (contact with floor).
{Fascia is a thin sheet or band of fibrous connective tissue separating or binding together muscles and organs}
Synonyms
- Plantar Fasciiosis (Because inflammation plays a lesser role, it is a disorder of the insertion of the ligament on the bone characterized by minor tears, breakdown of collagen and scarring)
- Jogger’s heel
How does Plantar Fasciitis happen?
- It is caused by excessive straining the ligament located at the bottom of your foot and supports your arch.
- When the fascia gets repeatedly strained, tiny tears occur in it.
- These tears can cause pain and swelling.
Causes
Exact cause is not understood well.
Under normal conditions, plantar fascia acts like a shock absorbing bowstring supporting arch of the foot. If the tension on that bowstring becomes too great, it can create small tears in the fascia. Repetitive stretching and tearing can cause the fascia to become irritated or inflamed.
Normally when we walk, the plantar fascia stretches as our foot strikes the ground. But if the fascia is strained by the way you walk or by repeated stress, it tends to become weak, swollen and irritated (inflamed) and it can hurt you when you stand or walk.
Below said are the conditions or activities that may lead to plantar fasciitis:
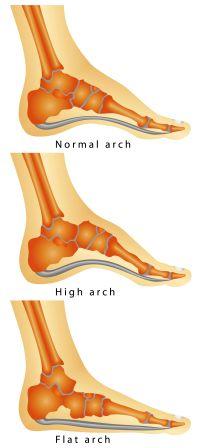
Bio-mechanical factors – factors that affect how the feet works.
- Plantar fasciitis may occur when your feet roll inwards too much when you walk (excessive pronation)
- High arches and flat feet – If you have high arches or flat feet you are in the risk of damaging your plantar fascia
- Being overweight
- You wear shoes that don’t fit well or are worn out
- Having tight Achilles tendons- When the tendons at the back of your heel are too tight it may strain the plantar fascia
- Having tight calf muscles can also predispose to Plantar Fasciitis
Repetitive activities: Jobs that require prolonged walking or standing on hard or irregular surfaces or sports such as running
Natural processes: Ageing, plantar fasciitis is more common in middle aged adults
Injury:Injury to the foot or directly over the fascia can cause plantar fasciitis by damaging the fascia
Symptoms
What are the symptoms of Plantar Fasciitis?
Classic symptom – Heel Pain, you may experience a stabbing pain in the bottom of your foot near the heel
When plantar fasciitis occurs, the pain is typically sharp and usually unilateral (70% cases)
- You will experience the pain when you get out of your bed and take first few steps or
- You will notice pain after sitting for a long period
Other symptoms (Nature of pain):
- Stiffness and pain in the morning or after resting, the pain gets better after taking a few steps.
- Your foot may hurt as the day progresses
- Foot may hurt the most when you climb stairs or after standing on your toes
- Pain after you stand for long periods
- Pain after sitting for a long time
- Pain is also brought on by bending the foot and toes up towards the shin
- Pain at the beginning of exercise that gets better or goes away as you continue your exercise. The pain returns back when you would have completed the exercise.
Note: If you have foot pain at night, you may have arthritis or a nerve problem such as tarsal tunnel syndrome
Rare symptoms:
- Numbness
- Tingling sensation
- Swelling
- Radiating pain
Rupture of plantar fascia (due to overuse of plantar fascia in the setting of plantar fasciitis), when present presents with:
- Clicking or snapping sound
- Significant local swelling
- Acute pain in the sole of the foot
What happens if Plantar Fasciitis progresses?
- Plantar Fasciitis usually develops gradually
- Initially you may have heel pain only when you take first steps after getting out of bed or sitting for a prolonged time as already said
- When this happens, you need to rest. The pain will get worse if you do not rest
- Repetitive stress of walking, standing, running or jumping will further add insult to injury, the pain and inflammation worsens with time
- If you do not stop the activity or change the condition which has caused pain and injury to your fascia, the injured ligament may never heal completely
When the plantar fasciitis progresses further, the below mentioned events might occur –
- Heel pain gradually gets worsened
- To avoid or relieve the pain, you may often change the way you walk. This eventually may lead to more discomfort and pain. Other problems may also be experienced in your foot, leg, hip or back. Gradually your involvement in many daily activities and sports may become even more limited.
- Any weight-bearing activity will bring on pain.
- Running and jumping will practically be impossible
- As a result of continued stress, a heel spur may be formed (as the plantar fascia pulls on the heel bone).
Note:
- A heel spur does not cause plantar fasciitis and does not usually cause problems. You can have a plantar fasciitis and not have a heel spur.
- Plantar fasciitis can cause constant and severe pain when you stand or walk if left unattended or untreated. Therefore it is wise to start treatment once the condition is diagnosed.
Preventive measures
Can I prevent Plantar Fasciitis?
Below mentioned are some of the steps which when followed helps you in preventing plantar fasciitis. If you already have plantar fasciitis, they will help the condition by preventing the progression towards worse. They are –
- Foot care – Take good care of your feet. Wear shoes with good arch support and heel cushioning. Stand on a rubber mat to reduce stress on your feet if your work demands standing on hard surfaces
- Stretching – Exercises to stretch the Achilles tendon at the back of your heel will help. They will not only help the sports people but also are handy in non-athletes. Request your doctor to recommend a stretching schedule
- Maintain weight – Maintain good and healthy weight in proportion to your height.
- Exercises – Make exercising a regular habit. Increase your exercise levels gradually and wear supportive shoes
- Run flip – Flip or alternate running with other sports that will not cause heel pain
- Shoe morning – Begin your morning by immediately putting on supportive shoes as soon as you are out of your bed. Going barefoot or wearing slippers puts stress on your foot and further damage them.
- Contact HRD – If you feel that your work activities caused your heel pain, ask your human resources department for information about different ways of doing the job that will not make your heel pain worse.
- Contact sports training specialist – If you are an athlete or a sports-person, it is better to consult a sports training specialist for training and conditioning programmes to prevent plantar fasciitis from recurring.
Risk factors
What are the risk factors of Plantar Fasciitis?
You are at a greater risk (greater chance of developing) of getting plantar fasciitis if you:
- Are middle-aged or older person. PF is most common in people between age-groups of 40 and 60 years
- Walk with an inward twist or roll of the foot (pronation)
- Have high foot arch
- Have flat foot
- Leg length inequality
- Are overweight
- Have tight Achilles tendons (tendons at the back of your heel, which attach your calf muscles to the heel bones)
- Have tight calf muscles (muscles at the back of your leg)
- Have habits or do activities that increase the stress on your feet such as:
Changing your walking or running surface (example – from grass surface to a harder surface like concrete surface)
- Having a job that involves prolonged standing on hard surfaces
- If you are an athlete or a member of the military
- Some athletes – especially runners are more likely to get plantar fasciitis because of:
Things that affect the way their feet strike the ground such as not having enough flexibility in the foot and ankle or having stronger muscles in one leg than in other
Improper training
- Activities: Ballet dancing, Dance aerobics
- Occupations – factory workers, teachers etc who spend a lot of time either walking or standing on hard surfaces
Runners and plantar fasciitis:
- If you are a runner, the chances of you getting plantar fasciitis if you:
- Abruptly change how hard or how long you run
- Run on steep hills
- Wear running shoes that do not have a cushioned sole, lack good arch support or shoes which are worn out
Complications
- Ignoring plantar fasciitis may result in chronic heel pain that hinders your regular activities
- You might also develop foot, knee, hip or back problems if you change the way you walk to minimize plantar fasciitis pain
Till when should I wait before calling the doctor?
When you have heel pain, wait and watch by doing the below said before calling a doctor or seeking medical help:
- Rest
- Stop or reduce activities that can cause pain (running, standing for long periods, walking on hard surfaces etc)
- Icing your heel
- Change shoes, use shoes with good arch support and well-cushioned soles, also try heel cups or shoe inserts to cushion your heel effectively
- Switch on to other activities that don’t put pressure on your heel. After the symptoms are gone, gradually resume the activities.
- If you are an athlete and have heel pain, do not ignore, don’t try to run in spite of having pain. This will lead to chronic problems which become difficult to handle
When should I see my doctor?
Doctor will help you with finding the cause, diagnosing the exact disease and appropriate treatment. is the perfect person to make a right diagnosis. The earlier your doctor diagnoses and treats the condition, the sooner you will be relieved of your pains.
Call your doctor if you have:
- Pain that continues when you are not standing or bearing any weight on your heel
- Heel injury that results in pain when you put weight on your heel
- Heel pain that is not getting better even after a week, in spite of you trying many sorts of easy remedies like rest, ice application, over-the counter medicines (pain killers) like ibuprofen or acetaminophen and other home treatments
- If you have been diagnosed with plantar fasciitis and the home treatment which the doctor had advised and you have been following is no longer helping you to get rid of the pain
- If the pain is associated with fever, redness or warmth, numbness, tingling sensation in the heel.
Pathophysiology
Originally, plantar fasciitis was believed to be an inflammatory condition of the plantar fascia. In the later periods, the studies have observed microscopic anatomical changes indicating that the plantar fasciitis is actually due to a non-inflammatory structural breakdown of the plantar fascia rather than an inflammatory process.
Therefore it was thought to be reasonable enough to name this condition as plantar fasciiosis rather than plantar fasciitis.
- The structural breakdown of the plantar fascia is believed to be the result of repetitive micro-trauma (small tears).
- Microscopic examination – of the plantar fascia often shows myxomatous degeneration, connective tissue and calcium deposits and disorganized collagen fibers
- Windlass mechanism – Disruptions in the plantar fascia’s normal mechanical movement during standing and walking known as Windlass mechanism are believed to contribute to the development of plantar fasciitis by placing excess strain on the calcaneal tuberosity
- Other studies – have shown that plantar fasciitis is not actually due to inflammed plantar fascia but may be a tendon injury involving the flexor digitorum brevis muscle located immediately deep to the plantar fascia
Diagnosis
Clinical examination: Diagnosis is usually done after considering the person’s history, risk factors and clinical examination.Your doctor will carry out a physical examination which includes checking your feet and watching how you stand and walk
They may interrogate you regarding:
- About your foot pain, its symptoms, location of pain, time of the day when the foot hurts the most, nature of the pain etc
- Your past health, illnesses and injuries
- The type of physical activities you are involved in, and how active you are
Findings at clinical examination:
- Tenderness along the inner aspect of the heel bone on the sole of the foot on palpation may be elicited.
- Foot may have limited dorsi-flexion due to tightness of the calf muscles or the Achilles tendon. Dorsi-flexion (backward bending) of the foot may elicit pain due to stretching of the plantar fascia with this motion.
Diagnostic Imaging:
Diagnostic imaging studies are not usually needed
- In some cases the physician may decide to go with imaging studies such as X-rays, diagnostic ultrasound or MRI to rule out serious causes of foot pain (like fractures, tumours or systemic disease – if pain fails to respond to conservative medical treatments)
- Bilateral heel pain or systemic illness related heel pain – may need more detailed investigations. In such cases, diagnostic tests like CBC or serological markers of inflammation, infection or autoimmune disease such as C-Reactive protein, ESR, ANA, RA factor, HLA-B27, uric acid or Lyme disease antibodies may also be obtained
- If there are neurological deficits along with fasciitis, EMG to evaluate for damage to the nerves and muscles may be required
X-rays:
- X-rays are not helpful in diagnosing plantar fasciitis as they do not show the ligaments clearly
- Your doctor may still advise you to take an X-ray of foot to rule out stress fractures, bone cysts and other foot/ ankle related bone problems.
- X-ray may show the presence of a heel spur, but its presence does not necessarily prove that a person has plantar fasciitis
Differential Diagnosis
Calcaneal stress fracture – presents with:
- Pain on inner or outer aspect of the heel pain
- Pain increases with impact activity like marching, running, jumping or landing
- In severe cases, walking aggravates pain
- Night pains
- Pain on firmly touching or squeezing the heel bone
Calcaneal bursitis – presents with:
- Back of ankle and heel pain
- Pain is experienced during walking, going up and down stairs, running, jumping or hopping
- Often pain may become worse at rest after these activities
- Limp in severe cases
- Tenderness on firmly touching the affected bursa
- Swelling around Achilles tendon area
Osteo-arthritis of foot and ankle – presents with:
- Pain or tenderness
- Reduced ability to move, walk or bear weight
- Stiffness in the joint
- Swelling in the joint
Spinal stenosis involving nerve roots of lumbar spinal nerve 5 (L5) or sacral spinal nerve 1 (S1) – presents with
- Sciatica – Pain, tingling, cramping and numbness in the low back area extending along the course of the sciatic nerve, down the lower limb along the buttock, back of thigh and leg and reaching to bottom of the foot and toes
Calcaneal fat pad syndrome – presents with:
- Pain in the heel, usually a deep, dull ache that feels like a bruise on the middle of the heel (plantar fascia pain or heel spur pain is normally present at the front of the heel, not the middle)
- Walking barefoot on hard surfaces like ceramic tile, concrete, hardwood floors, etc, aggravates the pain
- Pressing with your thumb into the centre of the heel should re-create the pain
- Condition can often be attributed to a blow to the heel – i.e. landing hard, stepping on a stone while running etc.
Seronegative spondyloarthropathies like
Reactive arthritis (ReA or Reiter syndrome)
Autoimmune condition that develops in response to an infection, associated with gastrointestinal infections like Shigella, Salmonella, Campylobacter, etc as well as genitor-urinary infections especially Chlamydia trachomatis
Presents with a classical triad of symptoms:
- Non-infectious urethritis
- Arthritis
- Conjunctivitis
Ankylosing spondylitis
It is a type of arthritis that affects the spine. It presents with –
- Constant pain and stiffness in the low back, buttocks and hips
- Bony fusion – abnormal joining of the bones affecting bones of hip, back and neck, may impair person’s ability to perform daily activities
- Pain in ligaments and tendons – causing pain and stiffness in the area behind and beneath the heel such as the Achilles tendon
Rheumatoid Arthritis of ankle joint and foot – presents with
- Pain
- Swelling
- Stiffness
- Instability
- Bone spurs
- Joint deformity
- Difficult walking
- Numbness
- Tingling sensation
- Development of bunions, metatarsalgia and hammertoes
Plantar fascia rupture – presents with:
Rupture of plantar fascia (due to overuse of plantar fascia in the setting of plantar fasciitis), when present presents with:
- Clicking or snapping sound
- Significant local swelling
- Acute pain in the sole of the foot
Compression neuropathies like
Tarsal nerve syndrome: – Also called posterior Tibial Neuralgia – presents with-
- Tingling, burning or a sensation similar to an electric shock
- Numbness
- Pain, including shooting pain
Impingement of medial calcaneal nerve – presents with:
- Burning pain below the medial malleolus (bony bit on the inside of the ankle)
- Pain may radiate under the sole of the foot
- Activities such as running etc will usually aggravate the condition
- Tenderness around the medial malleolus
- Positive Tinel’s test
Plantar fasciitis treatment:
The goals of treatment of plantar fasciitis are to:
- Relieve pain and inflammation in the heel
- Heal the small tears in the plantar fascia
- Improve strength and flexibility, correct foot problems such as excessive pronation so that you don’t stress the plantar fascia ligament
- Allow you to resume your normal activities as soon as possible
Ayurvedic aspects of Plantar Fasciitis
Without going into exact comparison and correlation technology, we can just put Plantar Fasciitis into the category of foot related pathological conditions explained in Ayurvedic texts, especially in the context of Vata Vyadhi (chapter dealing with diseases manifesting due to morbid Vata).
The below said are the foot related conditions explained in Vata Vyadhi chapter of Ayurveda:
Padakantaka
न्यस्ते तु विषमे पादे रुजः कुर्यात्समीरणः।
पादकण्टक इत्येष विज्ञेयस्तलमाश्रितः॥{यो.र.वा.व्या}
When we strain our foot by regularly working or walking on rough and uneven surfaces,the Vayu located in the foot gets disturbed and causes a painful condition at the base (bottom/plantar area) of the foot. This condition is called Padakantaka
This condition seems to be the most appropriate and closer comparison which can be made with the clinical picture of plantar fasciitis
Vatakantaka
रुक्पादे विशमे न्यस्ते श्रमाद्वा जायते यदा।
वतेन गुल्फमाश्रित्य तमाहुर्वातकण्टकम्॥{अ.सं.नि.१५}
Walking with foot placed on hard, odd and uneven surfaces and exertion (physical activities which demands running, jumping, walking much and involving sports and games) leads to the aggravation of Vayu.
This vitiated (morbid) Vayu gets located in the Gulpha (ankle and foot) and produces a painful condition of the foot. This is called Vatakantaka.
This condition seems to be a variant of Padakantaka but this is an extended version wherein the ankle joint too is involved along with foot. This too seems to be an apt comparison to plantar fasciitis especially when the causative factors are taken into consideration
The below said conditions also can be considered closer to the clinical picture of plantar fasciitis:
Padadaha
पादयोः कुरुते दाहं पित्तासृक्सहितोऽनिलः।
विशेतश्चङ्क्रमते पाददाहं तमादिशेत्॥{सु.नि.१}
Due to excessive walking and straining the foot, the morbid Vata gets associated with morbid pitta and rakta and causes burning sensation in the foot. This condition is called Padadaha.
Though pain is not a predominant feature of Padadaha, burning sensation can be considered as a type of pain and discomfort caused due to the involvement of morbid pitta and rakta along with morbid vata. But since vata is involved and this condition is explained in Vata Vyadhi chapter, we cannot ignore the predominant symptom caused by morbid vata i.e. pain.
We can consider that pain would be a main complaint very earlier in the disease when only Vata is vitiated and in later condition when it gets the association of morbid pitta and rakta, burning sensation – which is a hallmark feature of pitta (inflammation), occurs and masks the pain of vata. Burning sensation probably marks the progression of inflammatory process in the fascia.
Since the causative factor is excessive walking and straining of foot, Padadaha also can be categorized under Plantar Fasciitis. Moreover, burning symptom too is one of the symptoms narrated by patients suffering from plantar fasciitis
Padaharsha
हृष्यतश्चरणौ यस्य भवतस्तु प्रसुप्तवत्।
पादहर्षः स विज्ञेयः कफवातप्रकोपजः॥{सु.नि.१}
When the morbid Vayu gets the association of morbid kapha and gets lodged in the foot, they cause tingling sensation and numbness in the foot. This condition is called Padaharsha
We know that both these symptoms are part and parcel of plantar fasciitis
Khalli
खल्ली तु पाद जङ्गोरुकरमूलावमोटनी॥{च.चि.२८}
Khalli is a disease caused due to the morbid Vayu afflicting the foot (ankle), legs (knee), thigh (hip joint) and hand (wrist) causing severe painful cramps.
If we consider a part of the disease and look at the ‘cramps in foot and ankle’ Khalli appears closer to plantar fasciitis. Khalli cannot straightaway be compared with plantar fasciitis because it has an extension in terms of involvement of other joints too (not limited to foot). Cramping could follow excessive straining on foot and subsequent trauma.
We have learnt that injury is the main causative factor of plantar fasciitis. Injury (abhghata) is also one of the leading causative factors for the vitiation of Vata in the body.
Ayurvedic treatment
Treatment options of plantar fasciitis in Ayurveda:
Management of plantar fasciitis in Ayurveda involves –
- Nursing the injuries in the fascia with some effective treatments
- Taking control over the morbid doshas, especially Vata and Pitta
- Relieving the pain, inflammation and other symptoms associated with plantar fasciitis
- Treating on the lines of the above explained foot related pathologies as explained in Ayurveda
- Treatment on the lines of Vatarakta / Vatashonita Chikitsa (Treatment for Gout / Inflammatory or crystal arthritis) can be done in plantar fasciitis. Vatashonita is a disease manifested by the combined effect of morbid Vata and Rakta. This disease too starts manifesting by having its roots in the foot and when localized in foot and heels (plantar fascia), provides similar clinical picture.
Effective treatments:
Bahya / Sthanika chikitsa (External treatments):
Abhyanga (medicated massages) / Samvahana (soothing medicated massages) –
Massage of the foot and heel with medicated oils is always a preferable and convenient option in relieving pain and inflammation instantly. Patients will start feeling better right from the first sitting itself.
Padabhyanga (foot massage) is a specialty of Ayurveda. Pada or foot is said to be an important Karmendriya (motor organ of locomotion) without which we cannot carry on our daily activities. Foot health is important for our daily activities to go on smoothly and is hooked up with the main health. Guess doing some important work when your foot is painful?
Since foot is in the lower portion of the body, it is under the governance of Vayu. Vayu carries all the activities of the foot just like it carries the activities of the whole body. Thus the normalcy of Vayu is a must for a good foot health. Vayu can get strained when foot is strained due to vigorous activities and exercises and cause painful condition. It can thus cause pain in the foot and whole of the lower limb, vayu too gets aggravated with injury. Thus in plantar fasciitis, vata vitiation takes place on the back drop of abhighata or injury.
When Vayu gets disturbed it can pull or push things. When it pulls Pitta downwards from its site (ashayapakarsha), it can cause inflammation in the foot, ankle and plantar fascia, just like it causes elsewhere. When it pulls Kapha downwards, it causes symptoms like heaviness, stiffness etc.
Regular Padabhyanga is said to prevent many diseases including Sciatica and other foot related diseases.
Thus Padabhyanga is useful in prevention as well as treating the foot related pathologies, in fact application, pouring and anything which is done over foot with oil is beneficial in foot pain, because Taila or oil is the best remedy for Vayu. Ghrita or medicated ghee can also be mixed with the oil for better results in case of association of Pitta and Rakta.
Care should be taken in not giving a hard or deep massage. The pain and inflammation may worsen by doing so. Samvahana or soothing massages without application of pressure is the best option in dealing with plantar fasciitis.
Care should also be taken in choosing the medicament (medicated oil or ghee or both) for massage or pouring as in dhara.
Dhara: Stream pouring of medicated oils / ghee / decoction/ milk etc
- Sneha dhara: In this medicated oils / ghee / oils and ghee are poured over the affected part for a fixed schedule of time period. Samvahana can be simultaneously done. The oil can be used as such or made lukewarm. Too much heat can aggravate inflammation.
- Ksheeradhara: Medicated milk (milk processed with herbal drugs which have analgesic and anti-inflammatory properties or with decoctions prepared from the same drugs) is poured in streams over the affected part just is in Sneha Dhara. Milk processed with Dashamula, Laksha, Bala etc provides good relief.
Note: Dhara is usually done after Abhyanga or Samvahana with suitable oils
Avagahana: Foot dip in herbal oils:
A foot dip or immersion is given to the afflicted part. The patient is asked to dip his or her afflicted foot in herbal oils or processed milk (explained above).
Medicines used for Abhyanga, Dhara and Avagaha:
- Murivenna
- Ashwagandhabala Lakshadi Taila
- Mahanarayana Tailam
- Ksheerabala Tailam
- Prabhanjanavimardana Tailam / Kuzhampu
- Pinda Tailam
- Kottamchukkadi Tailam
- Sahacharadi Tailam
- Dhanwantaram Tailam
- Guggulutiktakam Ghritam etc
Lepa – Application of herbal pastes
Pastes prepared using the below said herbal powders can be used as applicants:
- Rasnadi churnam
- Kottamchukkadi churnam
- Grihadhumadi churnam
- Ellumnishadi churnam
- Jatamayadi churnam etc
Upanaha / Bandhana: Poultices and Bandaging
Poultices prepared by combining the above said churnas (mentioned in lepa) and oils mentioned in the context of Abhyanga can be used for applying analgesic and anti-inflammatory poultices. Bandages around the painful part too are helpful.
Ishtika Sweda (Brick fomentation)
This is one of the special treatments explained in Ayurveda which is extremely helpful in foot related pathologies like plantar fasciitis or calcaneal spur.
How is it done?
- A couple of bricks are heated red hot
- Herbal decoctions like Dashamula Kashayam are poured over the brick
- The affected part (foot) is massaged with herbal oils
- The foot is exposed to the fumes coming from the brick
- The procedure is repeated for 5-6 times and can be done once or twice daily
- The patient can also keep his foot on the brick covered in a sterile cloth once the heat of the brick is reduced
Abhyantara Chikitsa: Internal Treatment –
Virechana – Therapeutic purgation to eliminate morbid pitta and vata from the system and aid healing
Nitya virechana or daily purgation can be given with –
- Nimbamritadi Eranda Tailam
- Gandharvahastadi Eranda Tailam
- Sukumara Ghritam
- Avipatti Churnam
- Trivrit Leham
- Sukumara Leham etc
Vasti – Enemas
Enemas with medicated herbal oils (Matra vasti or Anuvasana Vasti) and medicated milk (Ksheera Vasti) are extremely beneficial in healing the pain and inflammation of plantar fasciitis.
The below said enemas are highly effective:
- Ksheera Vasti with Dashamula siddha ksheera (milk processed with Dashamula)
- Anuvasana or Matra Vasti with Guggulutiktaka Ghritam, Tiktaka Ghritam, Ksheerabala Tailam, Dhanwantara tailam, Dhanwantara Ghritam, Sahacharadi Tailam etc
Simple tests to identify the involvement of morbid Dosha in Plantar Fasciitis:
- If morbid Vayu is involved – Pain is predominant along with numbness, tingling sensation etc
- If morbid Pitta is involved – Burning sensation is predominant
- If morbid Kapha is involved – Stiffness is predominant
We know that alternate heat and cold application is a useful remedy in plantar fasciitis like alternating with ice and warm water application. We also know that heat application can aggravate plantar fasciitis symptoms in a few patients. In such patients we should consider the vitiation of Pitta and go ahead with cold application.
Abhyanga, Avagaha, Sweda, Dhara etc should be done without heating the oil / ghee/ milk too much. Lukewarm oils will help to an extent but not hot.
If heat application or treatments involving heat provides relief in plantar fasciitis it indicates towards involvement of morbid Vayu and / or Kapha, because for Vayu and Kapha which are basically cold in nature, heat application is antagonistic.
Ayurvedic medicines
Kashaya’s (Herbal decoctions):
- Guggulutiktakam Kashayam
- Sahacharadi Kashayam
- Sahacharabaladi Kashayam
- Kokilaksham Kashayam
- Rasnasaptakam Kashayam
- Guluchyadi Kashayam
- Gandharvahastadi Kashayam
Ghritam and Tailam (medicated ghee and oils):
- Guggulutiktakam Ghritam
- Varanadi Ghritam
- Rasnadi Ghritam
- Dhanwantaram Ghritam
- Tiktakam Ghritam
- Ksheerabala Tailam
- Sahacharadi Tailam
- Ksheerabala tailam 101
- Dhanwantaram tailam 101
Vati and Gulika (Tablets):
- Kaishora Guggulu
- Yogaraja Guggulu
- Panchatikta Ghrita Guggulu
- Ksheerabala Tailam 101 caps
- Dhanwantaram Tailam 101 caps
- Mahavata vidhwamsini Rasa etc.
External applications:
The same herbal oils mentioned in Abhyanga etc. can be used for external application.
Shatadhouta Ghritam is one of the excellent applications for plantar fasciitis. It is available in the form of medicated ghee or ointment. It is excellent in relieving pain, inflammation and other associated symptoms.
Jatyadi Ghritam / Tailam has a similar healing impact.
You have the best remedies for plantar fasciitis in Ayurveda but don’t forget to consult an Expert Ayurveda Doctor for an opinion before starting on with anything.
Allopathic treatment
- Pain killers – Take analgesics like Ibuprofen or Naproxen. NSAID’s are available in the form of pills and creams. They help in relieving pain and inflammation.
- Surgery: very early in the disease, you may not need surgery. Surgery is suggested only when other non-surgical treatments have failed to provide good relief even after a period of 6-12 months and when the heel pain is restricting your daily activities. 95% of patients get relieved of heel pain without surgery.
Main types of surgery for plantar fasciitis –
Plantar fascia release – This procedure involves cutting a part of the plantar fascia ligament. This releases the tension on the ligament and relieves the inflammation
Removing heel spur
Stretching or loosening specific foot nerves
Note: Heel spurs are the result and not the cause of plantar fasciitis
Other Treatments:
Physical therapy – It may be helpful for those having problems with foot mechanics (biochemical problems) such as a tight Achilles tendon along with plantar fasciitis
Extracorporeal Shock Wave Therapy (ESWT) – This form of treatment uses pulsed sound waves to treat plantar fasciitis. Studies show that ESWT can reduce symptoms of plantar fasciitis which have been otherwise stubborn to other treatments. Another variant called focused ESWT requires to be done under anaesthesia. Radial ESWT can be done without using anaesthesia
Iontophoresis – This involves applying anti-inflammatory substances such as dexamethasone or acetic acid topically to the foot and transmitting these substances through the skin with an electric current.
Novel treatments:
- Dry Needling (Myofascial Trigger Point Dry Needling) – is the use of either solid filiform needles (acupuncture needles) or hollow-core hypodermic needles for therapy of muscle pain, including pain related to myo-fascial pain syndrome
- Botulinum Toxin A injections
- Platelet-rich plasma injections
- Proltherapy (proliferation therapy or regeneration injection therapy) – includes injection an irritant solution into a joint space, weakened ligament or tendon insertion to relieve pain
Note:
- Plantar fasciitis pain will respond and reduce after a few weeks once you start on medication and lifestyle modifications. But the pain may continue for a longer course and take time to go away completely, say for about a few months to even years
- You need to stick on to the treatment, otherwise the pain may become more constant and consistent and make it difficult for you to stand or walk
Epidemiology
In who does Plantar fasciitis occur?
- Most common reason for heel pain responsible for 80% cases
- Tends to occur more in women, military recruits, older athletes, obese people and young male athletes
- In US alone, more than 2 million people receive treatment for plantar fasciitis. The cost of treating plantar fasciitis in US is estimated to be $284 million every year
- About 4-7% of people have heel pain at any given point of time and about 80% of these cases are due to plantar fasciitis
- Approximately 10% of people have the disorder at some point during their life
- Plantar Fasciitis is common in middle aged people
- It becomes more common with age
- It is also common in younger people who are always on their feet, like athletes or soldiers
- It can happen in one foot or both
- It is unclear if one sex is more affected than the other
Studies and Research
Relation between BMI and Plantar Fasciitis in non-athletes: There exists a strong association between an increased body mass index and the development of Plantar Fasciitis in the non-athletic population. This association between weight and plantar fasciitis has not been observed in the athletic population.
Plantar Fasciitis is non-inflammatory: The studies have observed microscopic anatomical changes indicating that the plantar fasciitis is actually due to a non-inflammatory structural breakdown of the plantar fascia rather than an inflammatory process.
Plantar Fasciitis is a tendon injury: Other studies have shown that plantar fasciitis is not actually due to inflamed plantar fascia but may be a tendon injury involving the flexor digitorum brevis muscle located immediately deep to the plantar fascia
What is the prognosis of plantar fasciitis?
- Most people completely recover within one year
- 95% of plantar fasciitis patients get relieved of their heel pain with non-surgical treatments
- Only 5% of plantar fasciitis patients might need the surgery
- The most successful step is when the treatment is started immediately after the symptoms are noted for the first time. It takes less time to provide pain relief. Early treatment is the key
- If the start of treatment is delayed it takes a lot of time to provide pain relief and might get stubborn with passage of time
References:
http://www.emedicinehealth.com/plantar_fasciitis-health/article_em.htm
http://www.uofmhealth.org/health-library/aa57571
https://en.wikipedia.org/wiki/Plantar_fasciitis
http://orthopedics.about.com/od/footankle/i/shockwave.htm








One comment on “Heel And Foot Arch Pain: Plantar Fasciitis Tips, Remedies”
sheejapaulos
Much obliged to you, for your amazing article on medicinal services guide. I was hunting through the net down when for such suitable article on medicinal services through Ayurveda. It has turned out to be an incredible help. Looking forward for some more related post.